When you walk down the street and suddenly your legs feel heavy, numb, or cramp up-so badly you have to stop and lean on a shopping cart just to catch your breath-you might think it’s just getting older. But if this keeps happening, especially when standing or walking, and gets better when you sit down or bend forward, it’s not normal aging. It could be neurogenic claudication, the most common symptom of lumbar spinal stenosis.
What Exactly Is Neurogenic Claudication?
Neurogenic claudication isn’t a disease on its own. It’s a set of symptoms caused by pressure on the nerves in your lower spine. As the space inside your spinal canal narrows-usually from years of wear and tear-the nerves that run down to your legs get squeezed. This leads to pain, tingling, weakness, or a heavy feeling in one or both legs, especially when you’re upright and moving. The key sign? Symptoms get worse when you’re standing or walking, and they get better when you sit down or bend forward. That’s why so many people with this condition end up leaning on shopping carts, walkers, or kitchen counters. It’s called the ‘shopping cart sign,’ and it shows up in 68% to 85% of confirmed cases. Some patients even report they can walk only 200 feet before their legs lock up-but push a cart, and suddenly they can go the whole grocery store. This is very different from vascular claudication, which comes from poor blood flow. With vascular claudication, pain goes away when you rest, no matter your posture. With neurogenic claudication, you need to bend forward. That’s why doctors ask specific questions: ‘Do you feel relief when you sit or lean forward?’ ‘Do you use a cart or walker to keep walking?’Why Does This Happen?
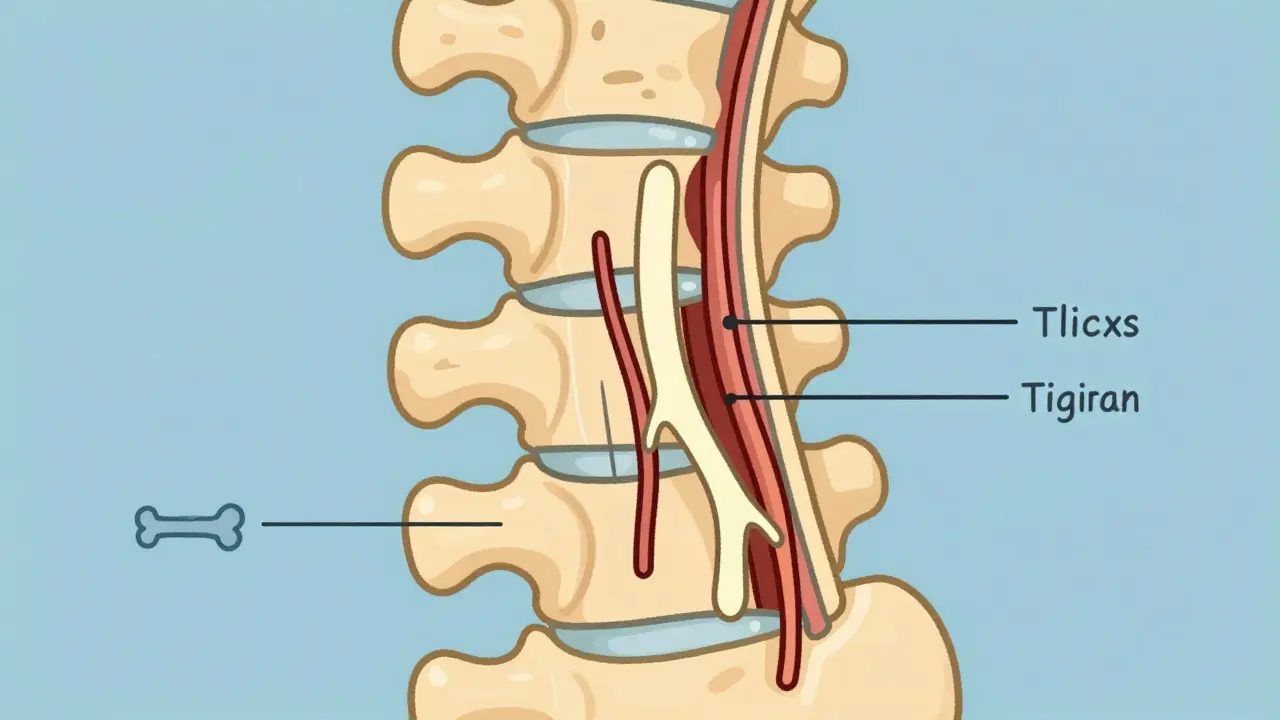
Lumbar spinal stenosis usually develops slowly. It’s tied to aging. Over time, the discs between your vertebrae dry out and flatten. Ligaments thicken. Bones and joints in your spine may grow extra bone (bone spurs). All of this crowds the space where nerves exit your spine. The pressure doesn’t just cause pain-it can also reduce blood flow to the nerves themselves. That’s why you don’t just feel sore muscles; you feel numbness, tingling, or even muscle weakness. In advanced cases, you might notice your foot muscles shrinking, especially the small muscles under your toes. Doctors call this bilateral extensor digitorum brevis wasting, and it’s a reliable clinical clue. It’s not just one spot that’s narrowed. Often, there’s central stenosis (the main canal is tight) and lateral stenosis (the side pathways where nerves exit are pinched). This dual problem makes symptoms worse and recovery harder.How Is It Diagnosed?
There’s no single test that confirms neurogenic claudication. Diagnosis is based on your story, your symptoms, and a physical exam. Your doctor will ask:- Do your legs hurt when you walk or stand for too long?
- Do you feel better when you sit down or bend forward?
- Do you use a cart or walker to keep walking?
- Do you feel weakness or numbness in your legs while walking?
What Are the Treatment Options?
Treatment follows a clear step-by-step path. Start simple. Only move to stronger options if things don’t improve.1. Conservative Management (First Line)
Most people find relief without surgery. The goal is to reduce pressure on the nerves and improve function.- Posture and movement: Learn to bend forward when walking. Use a walker or shopping cart. Avoid standing still for long periods.
- Exercise: Focus on flexion-based movements. Cycling (especially on a recumbent bike), swimming, and walking while leaning forward help. Avoid extension-heavy exercises like backbends or heavy lifting.
- Physical therapy: A therapist can teach you specific stretches and core strengthening moves. Most patients need 6 to 8 weeks of consistent therapy before seeing results.
- Pain relief: Over-the-counter NSAIDs like ibuprofen can help with inflammation. In some cases, doctors prescribe muscle relaxants or low-dose nerve pain meds like gabapentin.
2. Epidural Steroid Injections
If pain persists after 3 to 6 months of conservative care, injections may be considered. These deliver anti-inflammatory medicine directly around the affected nerves. Success rates vary-about 50% to 70% of patients get temporary relief, lasting from weeks to months. It’s not a cure, but it can buy time and reduce pain enough to keep doing physical therapy.3. Surgery (When Needed)
Surgery is considered when pain and weakness don’t improve after 6 months of conservative treatment, or if you’re losing strength or having trouble with balance. Common procedures include:- Laminectomy: Removal of the back part of the vertebra to open up space.
- Laminotomy: Partial removal-less invasive, good for single-level stenosis.
- Minimally invasive decompression: Smaller incisions, faster recovery. Newer devices like the Superion interspinous spacer (FDA-approved in 2023) hold the space open without removing bone.
What Happens If It’s Misdiagnosed?
This is where things go wrong. Many patients are told they have ‘poor circulation’ because their legs hurt when they walk. But if your pulses are strong and bending forward helps, it’s not vascular. One patient on Healthgrades said it took three doctors before someone asked, ‘Do you lean forward to feel better?’ Misdiagnosis leads to wrong treatment. You might get blood thinners or angioplasty for a circulation problem you don’t have-while your nerve compression keeps getting worse. That’s why accurate diagnosis matters so much. It’s not just about pain-it’s about preventing long-term nerve damage.What’s New in Treatment?
The field is evolving. In 2023, the American Academy of Orthopaedic Surgeons updated its guidelines to strongly recommend structured exercise as the first step-before injections or surgery. That’s a big shift. New minimally invasive tools like the Superion device are gaining traction. In trials, 78% of patients reported satisfaction two years after implantation. It’s not for everyone, but for some, it’s a game-changer. Researchers are also working on better diagnostic criteria. Right now, there’s no gold standard. The International Spine Study Group is finalizing a new algorithm expected in late 2024 to help doctors match symptoms more accurately to imaging findings.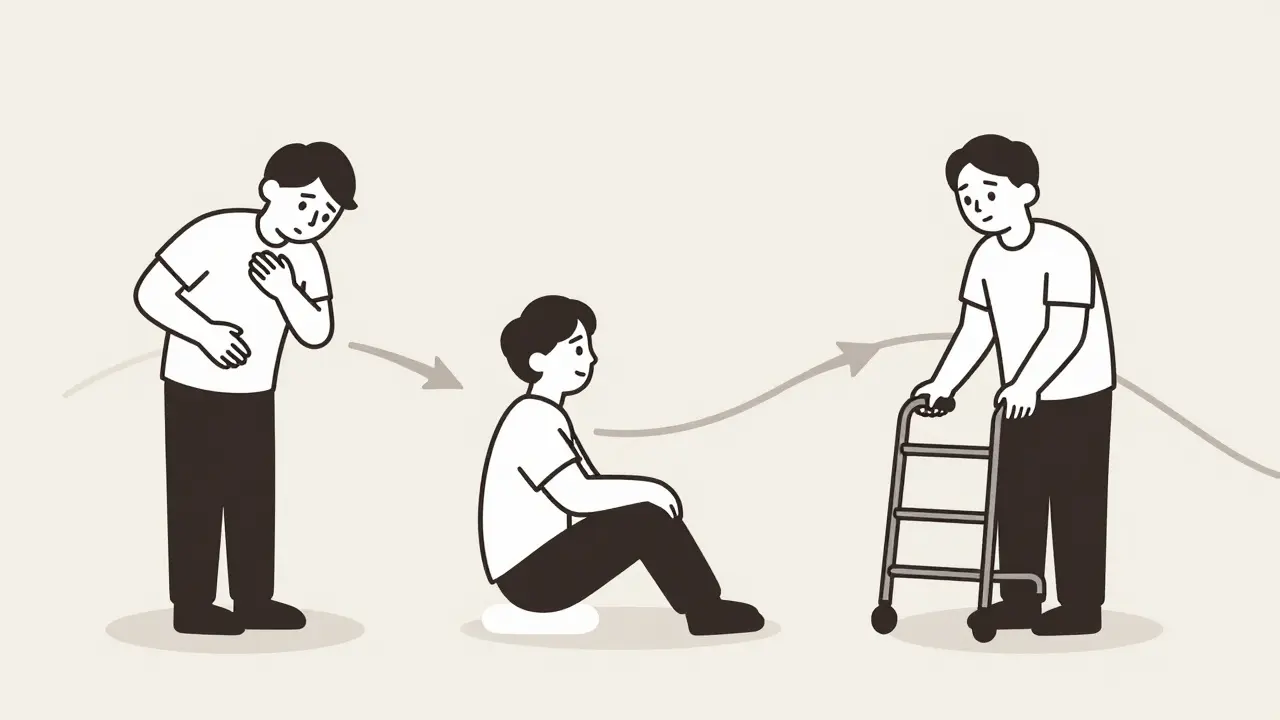
Living With It
This isn’t a condition you ‘beat.’ It’s one you manage. People who understand the ‘bend forward to relieve’ trick do better. One Reddit user wrote: ‘I used to walk 10 minutes and collapse. Now I push a cart, and I walk for an hour.’ Staying active matters. Even if you have to stop often, moving keeps your nerves healthy. Avoid prolonged sitting or standing. Use cushions or lumbar rolls to maintain a slight forward curve when sitting. The good news? You’re not alone. As the population ages, spinal stenosis is becoming more common. In the U.S. alone, about 200,000 adults are diagnosed each year. But with the right approach, most people keep walking-just differently.When to See a Specialist
See a spine specialist if:- Your leg pain or weakness is getting worse over weeks or months.
- You’ve tried physical therapy and pain meds for 3 to 6 months with no improvement.
- You’re having trouble with balance, or your feet feel like they’re ‘dragging’.
- You’ve lost bladder or bowel control (this is rare but urgent).
Is neurogenic claudication the same as sciatica?
No. Sciatica is pain that shoots down one leg, usually from a pinched nerve root-often due to a herniated disc. It’s sharp, electric, and often worse when sitting. Neurogenic claudication is more about heaviness, cramping, or weakness in both legs that gets worse with walking and improves with bending forward. Sciatica can be part of spinal stenosis, but not all claudication is sciatica.
Can I still walk with neurogenic claudication?
Yes, but you’ll need to adjust. Walking while leaning forward-using a walker, cart, or even a cane-helps open up space in your spine. Many people walk longer distances this way. Cycling on a recumbent bike is often easier than walking. The goal isn’t to stop moving-it’s to move smarter.
Do I need an MRI to confirm spinal stenosis?
Not always. Many people have narrowing on MRI with no symptoms. Diagnosis is based on your symptoms and exam. An MRI helps confirm the cause and rule out other issues, but it’s not the final word. If your symptoms match neurogenic claudication and you respond to conservative care, you may never need imaging.
Are epidural injections worth it?
For some, yes. About half to seven in ten people get relief that lasts weeks to months. It’s not a cure, but it can reduce pain enough to make physical therapy more effective. If injections help, they’re a bridge-not an endpoint. If they don’t work after two tries, surgery is often the next step.
Will I need surgery eventually?
Not necessarily. Most people manage well with conservative care. Surgery is only considered if symptoms are severe, worsening, or limiting daily life despite 6+ months of treatment. Even then, success rates are high-70% to 80% of patients feel much better after surgery. But it’s not for everyone. The decision depends on your symptoms, age, overall health, and how much it’s affecting your life.
Can neurogenic claudication come back after surgery?
Yes, but it’s uncommon in the first few years. The spine continues to age, and new narrowing can develop at other levels. Most patients who have good outcomes stay active and maintain core strength to reduce risk. Regular movement and avoiding heavy lifting help prevent recurrence.

