Every time you take an antibiotic, you’re not just fighting an infection-you’re also shaking up the trillions of bacteria living in your gut. Most people don’t realize that antibiotics don’t just kill the bad bugs. They wipe out the good ones too. And when those helpful microbes disappear, harmful ones like Clostridioides difficile (C. diff) can take over, leading to severe diarrhea, colitis, and even death. This isn’t just about one bad reaction. It’s part of a much bigger problem: antibiotic resistance.
What Is Antibiotic Stewardship?
Antibiotic stewardship isn’t a new buzzword. It’s a proven, science-backed approach to using antibiotics only when they’re truly needed-and using them the right way when they are. The CDC defines it as the effort to measure and improve how antibiotics are prescribed by doctors and taken by patients. It’s not about saying no to antibiotics. It’s about saying yes to the right antibiotic, at the right dose, for the right length of time. Think of it like this: if you use a sledgehammer to crack a nut, you’ll break the nut-and probably the table too. Antibiotics are powerful tools. But when they’re used too often, for too long, or for the wrong illness (like a cold or the flu), they damage more than they help.Why Antibiotic Overuse Is Dangerous
In the U.S., more than 2.8 million antibiotic-resistant infections happen every year. Over 35,000 people die from them. That’s more than car accidents or HIV/AIDS. And it’s not just hospitals. Outpatient clinics are major contributors. In fact, nearly half of all antibiotic prescriptions for acute respiratory infections-like bronchitis or sinus infections-are unnecessary. Why does this happen? Because it’s easier to write a prescription than to explain why antibiotics won’t help. Patients expect them. Doctors feel pressured. But here’s the truth: antibiotics don’t work on viruses. And most sore throats, coughs, and ear infections are viral. Giving an antibiotic in those cases does nothing for the patient-and everything for resistance. Each time you take an antibiotic unnecessarily, you’re helping bacteria evolve. The survivors become stronger. They pass on their resistance genes. Soon, the drugs that once saved lives stop working. And when that happens, even simple surgeries or chemotherapy become risky.How Antibiotics Damage Your Gut
Your gut is home to trillions of bacteria-most of them good. They help digest food, make vitamins, train your immune system, and keep harmful microbes in check. Antibiotics don’t distinguish between friend and foe. They sweep through like a tsunami. The most common consequence? C. diff infection. This bacteria lies dormant in many people’s guts until antibiotics wipe out the competition. Then it explodes. C. diff causes severe diarrhea, fever, and abdominal pain. In 2019, it led to over 223,900 infections and 12,800 deaths in the U.S. alone. And antibiotic use is the #1 risk factor. Studies show that about 20% of people who take antibiotics develop C. diff. That’s 1 in 5. And it’s not just a one-time problem. Once you’ve had it, your risk of getting it again is much higher. And recovery isn’t simple. Some people need fecal transplants just to restore their gut balance.
The Core Elements of Effective Stewardship
Successful antibiotic stewardship isn’t guesswork. It’s built on seven proven components, known as the CDC’s Core Elements:- Leadership commitment-hospitals and clinics must dedicate staff and resources.
- Accountability-someone must be in charge, usually an infectious disease doctor or pharmacist.
- Drug expertise-pharmacists trained in antibiotics guide prescribing.
- Actions-practices like switching from IV to oral antibiotics early, or shortening treatment duration.
- Tracking-measuring how many antibiotics are used (days of therapy per 1,000 patient days).
- Reporting-sharing data with prescribers so they see how they compare to peers.
- Education-teaching doctors, nurses, and patients why this matters.
What You Can Do as a Patient
You don’t need to wait for a hospital program to make a difference. Here’s how you can protect yourself:- Ask: “Do I really need this antibiotic?” If your doctor says yes, ask why. If they say no, ask what else you can do to feel better.
- Never take leftover antibiotics. A prescription meant for a past infection won’t help a new one-and might make it worse.
- Don’t pressure your doctor. If you have a cold or sore throat, don’t demand antibiotics. It’s not helping you-it’s hurting everyone.
- Complete the full course-if it’s truly needed. Stopping early can leave behind the toughest bacteria. But if your doctor says you can stop early (some infections now need only 3-5 days), follow that advice.
- Support gut health after antibiotics. Eat fermented foods (yogurt, kefir, sauerkraut), fiber-rich vegetables, and consider a probiotic with strains like Lactobacillus rhamnosus or Saccharomyces boulardii-both shown to reduce C. diff risk.
How Stewardship Saves Lives and Money
This isn’t just about health-it’s about cost. In U.S. hospitals, improper antibiotic use costs over $1 billion a year. But stewardship programs pay for themselves. A 444-bed hospital saved over $2 million annually by using handshake stewardship. They also cut C. diff cases by 30% and shortened patient stays. Outpatient clinics are catching on too. One study found that putting simple commitment posters in exam rooms-saying “I promise to only prescribe antibiotics when needed”-reduced inappropriate prescribing by 5.6%. That’s a small change with a big impact. By 2025, the CDC projects that widespread stewardship could prevent 130,000 C. diff infections and save 10,000 lives each year in the U.S. alone. That’s not a prediction. It’s a goal within reach-if we act now.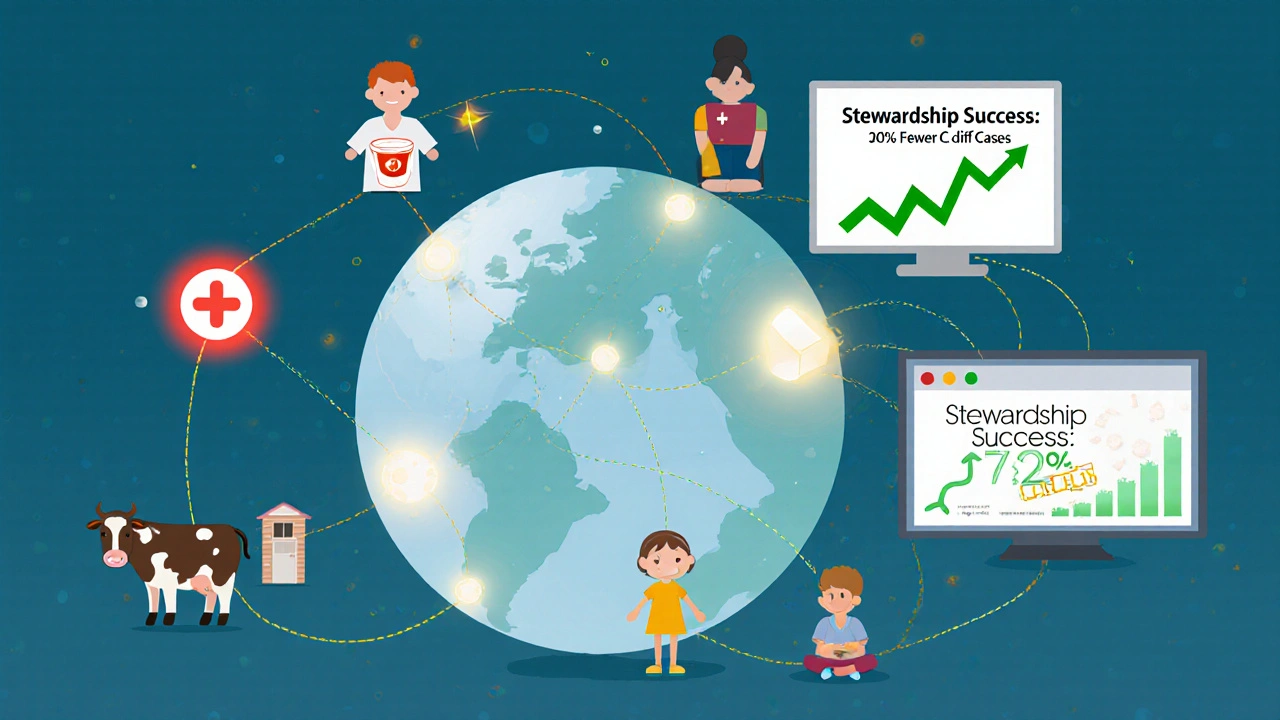
The Future: AI, Rapid Tests, and Better Tools
The next wave of stewardship is here. Hospitals are testing AI tools that analyze patient data in real time and suggest whether an antibiotic is likely needed. Some systems flag prescriptions before they’re even written. Early results show a 15-20% improvement in appropriate use. Rapid diagnostic tests are also changing the game. Instead of waiting 48 hours for a culture, new tests can identify bacteria and their resistance patterns in under two hours. That means doctors can switch from broad-spectrum drugs to targeted ones faster-reducing collateral damage to your gut. Pediatric guidelines updated in 2020 now recommend shorter courses for ear infections and sinusitis. For many kids, 5 days is enough-not 10. That’s a huge win for gut health.It’s Not Just a Hospital Problem
Antibiotic stewardship isn’t just for big hospitals. It’s needed in nursing homes, clinics, and even veterinary medicine. In fact, 70% of antibiotics sold globally are used in animals. That’s a major driver of resistance that affects human health. The good news? 84% of large U.S. hospitals now have formal stewardship programs. But only 54% of smaller hospitals do. And outpatient settings? Still lagging. That’s where the biggest opportunity-and risk-lies.Protecting Your Gut Is Protecting the Future
Antibiotics saved millions of lives. But they’re not magic. They’re tools-and like any tool, they wear out with misuse. Every unnecessary antibiotic you take chips away at their power. And every time you help preserve them, you’re not just protecting yourself. You’re protecting your children, your neighbors, and future generations. Your gut microbiome is a living ecosystem. Treat it with care. Ask questions. Push back gently. Choose evidence over expectation. And remember: the best antibiotic is the one you never need to take.Are antibiotics always necessary for infections like sinusitis or bronchitis?
No. Most sinus infections and nearly all cases of bronchitis are caused by viruses, not bacteria. Antibiotics won’t help and can harm your gut. The CDC estimates that 46% of antibiotic prescriptions for acute respiratory infections are unnecessary. Watch for symptoms that last longer than 10 days or worsen after improving-those might signal a bacterial infection needing treatment.
Can probiotics help after taking antibiotics?
Yes, certain probiotics can reduce the risk of antibiotic-associated diarrhea and C. diff. Strains like Lactobacillus rhamnosus GG and Saccharomyces boulardii have strong evidence backing them. Take them during and for a week after antibiotics, but don’t take them at the same time-space them 2-3 hours apart. Food sources like yogurt, kefir, and sauerkraut also help restore balance naturally.
Is antibiotic resistance really a personal problem?
Absolutely. Every time you take an antibiotic unnecessarily, you’re helping resistant bacteria survive and spread. These bugs don’t respect borders-they live on your skin, in your home, and can pass to others. When common antibiotics stop working, even minor cuts or routine surgeries become dangerous. Your choices affect your community.
How do I know if my doctor is practicing antibiotic stewardship?
Ask them. A stewardship-minded provider will explain why they’re prescribing (or not prescribing) an antibiotic. They’ll mention alternatives like rest, fluids, or pain relief. They won’t dismiss your concerns. If they say, “It won’t hurt to take it,” that’s a red flag. Good stewardship means saying no when it’s not needed-and saying yes with confidence when it is.
Can I prevent C. diff infection just by avoiding antibiotics?
Avoiding unnecessary antibiotics is the single best way to prevent C. diff. But even necessary antibiotics carry some risk. To lower it further, eat fiber-rich foods, stay hydrated, wash your hands regularly, and avoid proton-pump inhibitors (like omeprazole) unless absolutely needed-they raise C. diff risk too. If you’ve had C. diff before, talk to your doctor about preventive strategies before your next antibiotic course.


Comments (14)