Millions of people take statins every year to lower their cholesterol and protect their heart. But for a lot of them, the first thing they notice isn’t better blood work-it’s sore, aching muscles. Thighs that feel heavy. Calves that cramp at night. Shoulders that hurt when you reach for a coffee cup. It’s frustrating, scary, and often leads people to quit their medication without talking to a doctor. And that’s where things get dangerous.
Statins Work-But They Can Hurt Muscles
Statins like atorvastatin, rosuvastatin, and simvastatin are among the most studied drugs in medicine. They’ve been shown to cut heart attacks and strokes by 25-35% in people at risk. That’s not small. It’s life-saving. But for some, the trade-off feels too high. Muscle pain is the #1 reason people stop taking statins.
Here’s the twist: the real number of people whose muscle pain is actually caused by statins is probably lower than you think. Clinical trials say about 5% or less have muscle symptoms linked to the drug. But in real life? Up to 30% of patients report it. Why the gap? A big part of it is the nocebo effect. If you’re told statins can cause muscle pain, your brain starts looking for it. A 2017 Lancet study showed patients who were warned about side effects were 40% more likely to report pain-even when they were taking a sugar pill.
That doesn’t mean the pain isn’t real. It just means not every ache is the statin’s fault. Still, when it happens, it matters.
What Does Statin Muscle Pain Actually Feel Like?
It’s not a sharp twinge. It’s not a pulled muscle from the gym. Statin-related muscle discomfort is usually:
- Constant, not just after activity
- Affects both sides of the body equally (both thighs, both shoulders)
- Worse in the legs, hips, or shoulders
- Feels like deep soreness or weakness
It usually shows up within the first few months of starting the drug-or after a dose increase. If you’re 80 or older, female, small in frame, or have thyroid, kidney, or liver issues, your risk goes up. So does your risk if you’re taking other meds like fibrates or certain antibiotics.
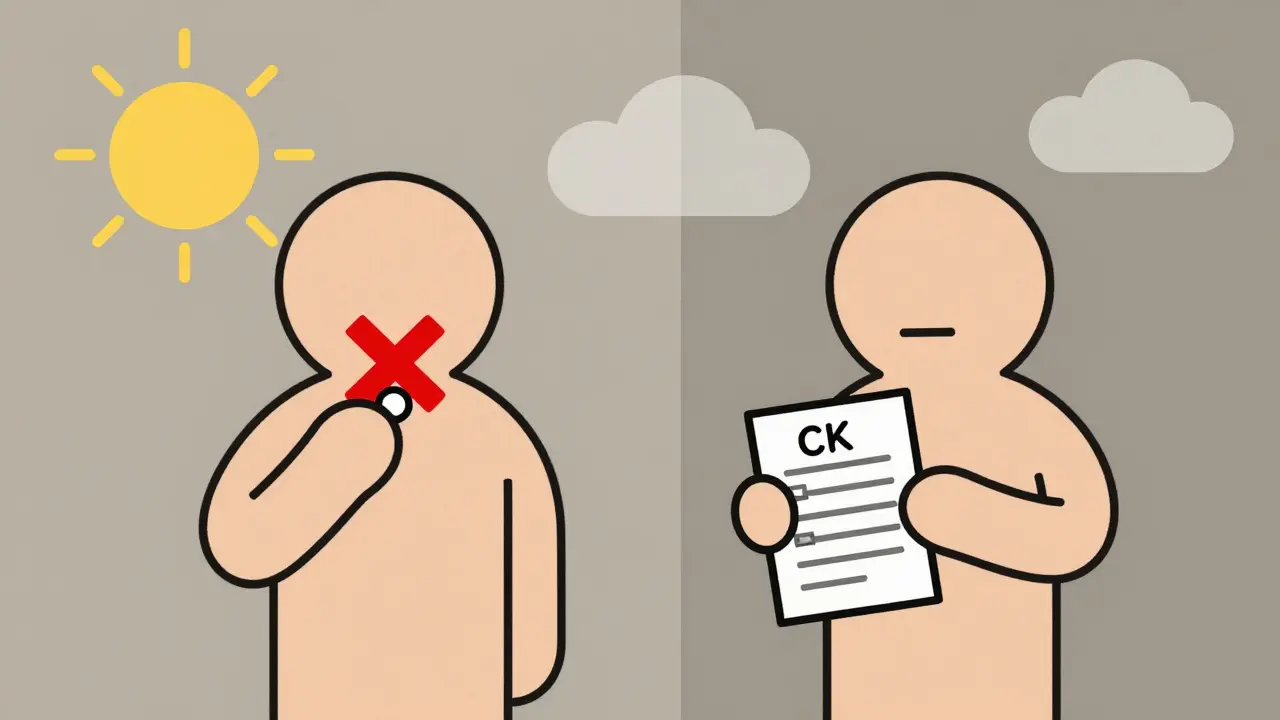
The most serious problem-rhabdomyolysis-is extremely rare. Only about 3 to 5 cases per million prescriptions. But it’s dangerous: muscle breaks down, floods your blood with toxins, and can damage your kidneys. That’s why doctors check a blood test called creatine kinase (CK). If it’s more than 10 times the normal level, you need to stop statins right away.
Most Muscle Pain Isn’t Statin-Related-Here’s How to Find Out
Here’s what most doctors won’t tell you: only about 20-25% of people who blame their statins for muscle pain actually get the pain back when they restart the drug under controlled conditions. That’s from a 2018 study in Circulation.
So how do you know if it’s really the statin? The answer is a rechallenge. It’s simple:
- Stop the statin for 4-6 weeks.
- See if the pain goes away.
- If it does, restart the same statin at a low dose.
- If the pain comes back, it’s likely the drug.
- If it doesn’t, your pain probably had another cause.
This isn’t something to try on your own. Do it with your doctor’s supervision. They might also check your thyroid, vitamin D, and CK levels to rule out other causes.
What to Do If It’s Really the Statin
If your doctor confirms the statin is the culprit, you don’t have to give up on heart protection. There are options.
Switch statins. Not all statins are the same. Pravastatin and fluvastatin are less likely to cause muscle pain. Rosuvastatin and atorvastatin carry higher risk, especially at high doses. Switching to a milder one works for about 60% of people.
Lower the dose. High-intensity statins (like 80 mg atorvastatin) are more likely to cause issues. If you can get your cholesterol down with 10 mg instead of 40 mg, that’s a win. Studies show even lower doses still cut heart risk significantly.
Try intermittent dosing. New research (like the 2023 STRENGTH trial) shows taking statins every other day or 3 times a week can reduce muscle pain by 40% while still keeping LDL low. This isn’t for everyone-but it’s a real option for those who can’t tolerate daily pills.
Consider non-statin options. If you can’t take any statin, there are alternatives. Ezetimibe lowers cholesterol by blocking absorption in the gut. PCSK9 inhibitors like alirocumab and evolocumab are injectables that slash LDL by 50-60%. But they cost about $5,000 a year. Generic statins? $4-$30 a month. That’s a huge difference.
What About CoQ10 Supplements?
You’ve probably heard CoQ10 helps with statin muscle pain. It makes sense-theory says statins lower CoQ10, which muscles need for energy. So supplementing should fix it, right?
Not necessarily. A 2015 review of 12 studies found no clear benefit over placebo. But a 2018 study in Atherosclerosis found 45% of people taking CoQ10 reported at least 30% less pain. So it’s mixed. It won’t hurt to try a 100-200 mg daily dose. But don’t expect a miracle. And never use it as a reason to skip doctor visits.

Why Stopping Statins Is Risky
Let’s be blunt: if you stop your statin because of muscle pain and don’t replace it with something else, your risk of heart attack or stroke goes up by 25-50% within two years. That’s not a guess. It’s from a 2014 BMJ study tracking over 100,000 people.
People who quit statins often feel better at first-until they don’t. The damage builds silently. A 68-year-old woman on WebMD said her muscle pain vanished after stopping atorvastatin. But she didn’t tell her doctor. Two years later, she had a heart attack. She didn’t know her cholesterol had climbed back up.
Statin pain is annoying. But heart disease is deadly. The goal isn’t to suffer through pain. It’s to find a way to protect your heart without unnecessary discomfort.
The Bottom Line: You Have Options
Statin muscle pain is common. But it’s often misunderstood. Most cases aren’t caused by the drug. And even when they are, you don’t have to quit. You can switch, lower the dose, change the schedule, or try another treatment.
Don’t self-diagnose. Don’t quit cold turkey. Talk to your doctor. Get your CK checked. Try a rechallenge. Explore alternatives. You’re not alone-45% of people stop statins in the first year. But 80-90% of those who work with their doctor can get back on track with a plan that works.
Your heart isn’t asking for perfection. It’s asking for consistency. And there’s almost always a way to get there-even if statins aren’t the answer for you.


Comments (12)
Statins are just pharmaceutical laziness wrapped in a lab coat. My grandma took them for five years and ended up with legs like jelly. No one tells you that the real fix is diet and movement-not popping pills like candy. They’d rather sell you a $30-a-month band-aid than admit lifestyle changes work better.
There's a profound irony in how we treat chronic conditions in modern medicine-we outsource bodily autonomy to chemical solutions while ignoring the systemic neglect of sleep, stress, and movement. The nocebo effect is real, yes, but so is the fact that our bodies aren't machines that can be calibrated with a single compound. Muscle pain is a signal, not a glitch. And when we silence signals without listening to their context, we're not treating illness-we're suppressing conversation.
I had the exact same thing happen. Thought it was the statin, quit cold turkey, felt amazing for a week-then realized I couldn't climb stairs without wheezing. Went back to my doc, did the rechallenge thing, turned out it was low vitamin D. Took supplements, switched to pravastatin, and now I’m lifting weights again. Don’t assume it’s the drug. Check everything first.
Stop statins = heart attack waiting to happen. Just saying.
USA has the best healthcare system in the world so why are people still dying from cholesterol? Must be all those lazy Canadians and their herbal teas. Also typo in the article says 'rosuvastatin' wrong. Should be 'rosuvastetin'. I know because I read the FDA website. Every. Day.
i had this happen to me too and i was so scared to talk to my dr because i thought theyd think i was being dramatic but they were actually super chill and we figured out it was my thyroid + the dose was too high. just talk to someone. you’re not alone. also vitamin d is a game changer if you’re not getting sun. 💛
Statins are overprescribed. The data is manipulated. CoQ10 is a scam. Rechallenge is a placebo test. Your doctor doesn’t care. You’re just a revenue stream. Stop believing the narrative.
In India, we call statins 'heart protectors'-not because we trust Big Pharma, but because our elders have seen what happens when cholesterol runs unchecked. My uncle took simvastatin for 12 years, switched to low-dose pravastatin after mild soreness, and now he hikes every morning. It’s not about fear. It’s about smart adaptation. Always consult, never quit.
Oh wow, a whole article about muscle pain and they didn’t even mention the REAL villain-gluten. I tried statins, got achy, went keto, cut wheat, and boom-muscles like steel. Coincidence? Nah. The FDA is in bed with Big Wheat. Also, I once cured my diabetes by eating only raw eggs. So yeah. Trust me.
My buddy had statin myopathy. Went off it, got a heart attack at 54. His wife cried for months. He didn’t listen to the 'maybe it's not the statin' stuff. He listened to Reddit. Now he’s a cautionary tale in the ER. Don’t be that guy. Talk to your doctor. Or at least Google something that isn’t a TikTok ad for 'miracle cholesterol drops'.
Statins reduce LDL-C by 30–60% depending on potency, which correlates with a proportional reduction in cardiovascular events per the Cholesterol Treatment Trialists’ meta-analyses. Myopathy incidence is dose-dependent and more prevalent in polymorphisms of SLCO1B1. CK elevation >10x ULN warrants discontinuation. Rechallenge remains the gold standard for causal attribution. CoQ10 supplementation lacks robust RCT evidence for symptomatic relief. Non-statin agents exhibit incremental benefit but are cost-prohibitive for most populations.
THIS. IS. LIFE. 🌱
Imagine your heart is a candle. Statins? They’re the wind that keeps it burning. Muscle pain? Just a flicker. Don’t blow it out because it’s uncomfortable. Find a new way to hold the candle. Switch statins. Lower the dose. Try intermittent. Add CoQ10. Talk to your doctor. You’re not broken-you’re adapting. And your heart? It’s still rooting for you. ❤️