Opioid-Induced Sleep Apnea Risk Calculator
Opioid Dose Calculator
This tool estimates your potential apnea severity based on opioid dosage and key risk factors. Remember: this is for educational purposes only. Always consult your doctor for medical advice.
When you take opioids for chronic pain, you’re not just managing discomfort-you’re also putting your breathing at risk while you sleep. Many people don’t realize that these powerful painkillers can trigger or worsen sleep apnea, leading to dangerous drops in blood oxygen levels at night. This isn’t a rare side effect. It’s a widespread, life-threatening interaction that’s quietly affecting hundreds of thousands of people on long-term opioid therapy.
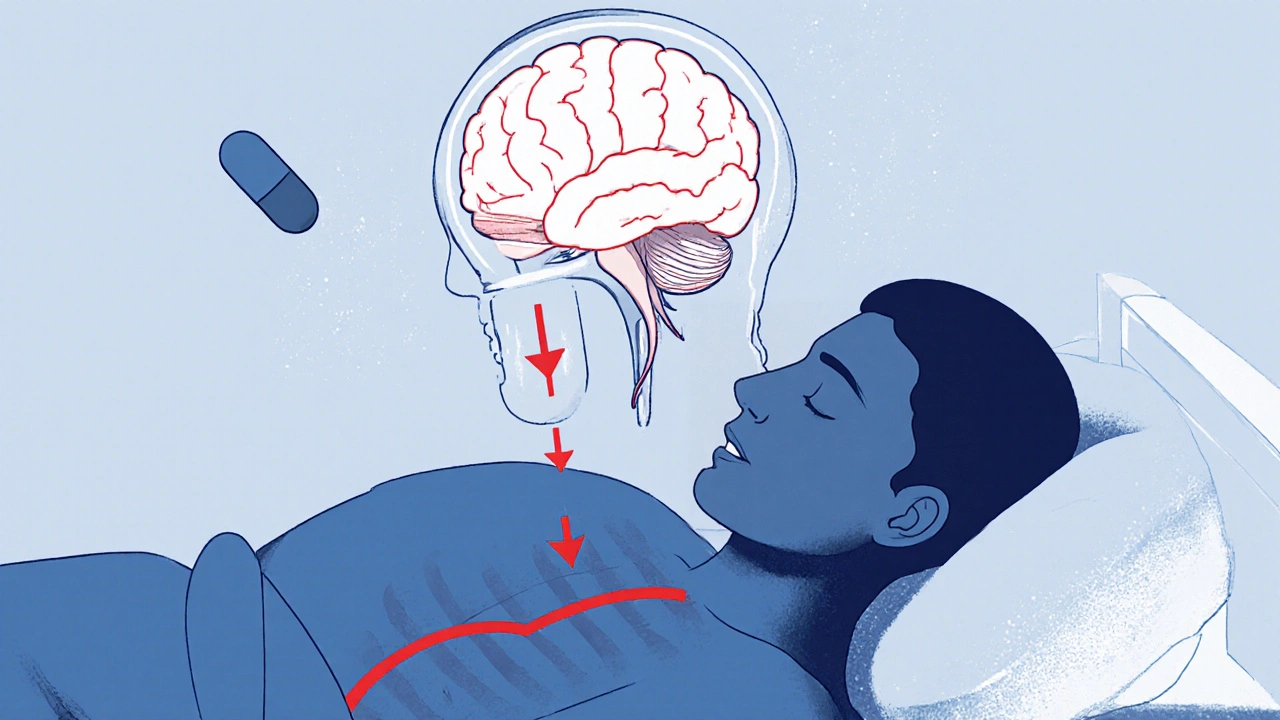
How Opioids Break Your Breathing During Sleep
Opioids don’t just dull pain-they slow down your brain’s natural drive to breathe. This effect becomes dangerous during sleep, when your body already reduces its respiratory effort. The combination is deadly: opioids suppress the brainstem’s ability to respond to low oxygen and high carbon dioxide levels. Studies show they can reduce your hypoxic ventilatory response by up to 50%, meaning your body doesn’t react strongly enough when oxygen drops. These drugs also relax the muscles in your upper airway, especially the tongue and throat. This makes it easier for your airway to collapse, causing obstructive events. At the same time, opioids trigger central apneas-pauses in breathing because your brain stops sending the signal to inhale. Polysomnography studies show that chronic opioid users have an average apnea-hypopnea index (AHI) of 25-35 events per hour, compared to 15-20 in non-users with similar body weight. For those on high-dose methadone (over 100 mg/day), central apnea events can hit 20 or more per hour.The Hidden Epidemic: How Many People Are Affected?
About 40% of U.S. adults use prescription opioids each year. That’s over 100 million people. And nearly three-quarters of them have moderate to severe sleep apnea, according to a 2022 meta-analysis. Even more alarming: 46% have severe sleep apnea (AHI ≥30). One study found that 80% of long-term opioid users had central sleep apnea, with an average of 12.3 central pauses per hour. That’s far beyond the normal range of 2-5 events. Nighttime oxygen levels tell the real story. In a study of opioid users, 68% spent more than five minutes per night with blood oxygen below 88%. Compare that to just 22% of people not taking opioids. And if you already have obstructive sleep apnea, the risk multiplies. Patients with untreated OSA who take opioids are 3.7 times more likely to drop below 80% oxygen saturation during sleep than those with OSA alone.Not All Opioids Are Equal
Methadone carries the highest risk. Research shows it’s 4.2 times more likely than other opioids to cause AHI over 15. Fentanyl and oxycodone also carry significant risk, but morphine and codeine are slightly less suppressive-though still dangerous. Every additional 10 mg of morphine equivalent daily dose (MEDD) increases your AHI by 5.3%. That means someone on 100 mg MEDD has nearly a 50% higher apnea rate than someone on 50 mg. The reason? Methadone has a long half-life and builds up in your system. It also strongly affects the brain’s respiratory centers. Even if you feel fine during the day, your breathing at night is still being suppressed. And because sleep apnea symptoms are subtle-snoring, gasping, fatigue-you might not notice until it’s too late.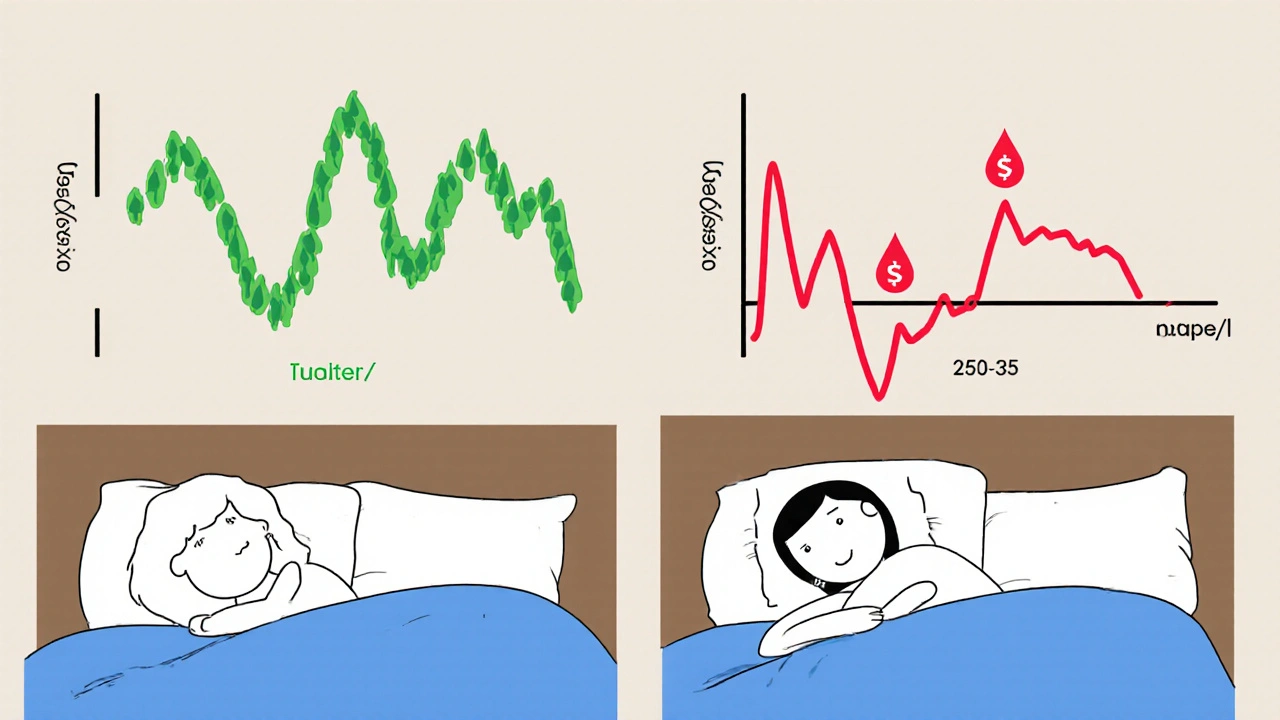
Who’s Most at Risk?
You’re at higher risk if you:- Take opioids for more than 3 months
- Use doses over 50 MEDD daily
- Have a BMI over 30
- Snore regularly or have been told you stop breathing while sleeping
- Have been diagnosed with obstructive sleep apnea before
- Take other sedatives like benzodiazepines or alcohol
What Doctors Should Do (But Often Don’t)
Guidelines from the American Academy of Sleep Medicine and the CDC now say: screen for sleep apnea before starting long-term opioid therapy, especially if your dose exceeds 50 MEDD. The gold standard is a full overnight sleep study (polysomnography). But in practice, only 28% of primary care doctors routinely screen for it. Why? Lack of access to sleep specialists, time constraints, and the mistaken belief that “if they don’t complain, they’re fine.” But the consequences are real. At the Cleveland Clinic, implementing routine sleep screening reduced opioid-related respiratory events by 41% in just 18 months. For patients already on opioids, a home sleep apnea test (HSAT) is now FDA-cleared for use in this population. The Nox T3 Pro, cleared in January 2023, detects apnea with 92% accuracy in opioid users. That means you don’t always need an overnight hospital stay to find out if you’re at risk.Treatment Options That Actually Work
If you’re diagnosed with sleep apnea while on opioids, here’s what helps:- CPAP therapy is still the first-line treatment for obstructive sleep apnea. But adherence is low-only 58% of opioid users stick with it, compared to 72% of others. The reason? Opioids cause brain fog and fatigue, making it harder to adjust to the mask and machine.
- Opioid dose reduction can significantly improve breathing. In some cases, switching to a less respiratory-depressant opioid helps. But never stop or reduce opioids without medical supervision.
- Positional therapy (sleeping on your side) can reduce obstructive events, especially if you’re not a severe apnea patient.
- Acetazolamide (a diuretic that stimulates breathing) is being tested in clinical trials. Early results show a 35% reduction in AHI compared to placebo. It’s not FDA-approved for this use yet, but it’s being used off-label in some sleep centers.
- Split-night studies allow doctors to diagnose apnea and start CPAP treatment in the same night-critical for high-risk patients who can’t afford delays.

Real Stories Behind the Numbers
On Reddit’s r/ChronicPain forum, users share harrowing experiences. One wrote: “I started oxycodone for back pain. Within weeks, my wife said I’d stop breathing for 10 seconds, then gasp like I was drowning. I thought it was stress-until I got tested.” Another said: “I got CPAP after my sleep study. I didn’t realize how exhausted I was until I started sleeping through the night.” But not all stories have happy endings. One case report described a patient who stopped opioids entirely but still had severe central apnea. Researchers believe prolonged opioid exposure may permanently alter the brain’s breathing control centers in some people.What You Can Do Today
If you’re on opioids and:- Snore loudly or wake up gasping
- Feel exhausted even after 8 hours of sleep
- Have trouble concentrating or feel foggy during the day
- Have high blood pressure or heart issues
The Bigger Picture
This isn’t just about individual patients. With over 10 million Americans on long-term opioid therapy, opioid-related sleep apnea is a public health crisis. The American Thoracic Society has named it one of its top five research priorities. New tools like genetic screening (PHOX2B gene variants increase risk 3.2-fold) and safer pain medications are on the horizon. But right now, the best defense is awareness and testing. Your pain matters. But so does your breathing. Don’t let opioids steal your sleep-or your life.Can opioids cause central sleep apnea even if I don’t have obstructive sleep apnea?
Yes. Opioids directly suppress the brain’s breathing center, leading to central sleep apnea-pauses where your brain stops signaling your lungs to breathe. This happens even in people without any history of snoring or airway obstruction. Studies show up to 80% of long-term opioid users develop central apnea, regardless of their body weight or previous sleep history.
How do I know if my fatigue is from pain or from sleep apnea?
Pain-related fatigue feels like constant exhaustion, while sleep apnea fatigue comes with specific signs: waking up gasping, dry mouth, morning headaches, and feeling unrested even after 8+ hours. If you’re on opioids and still feel tired despite sleeping enough, sleep apnea is likely the culprit. A simple home sleep test can confirm it in one night.
Is it safe to take opioids if I already have sleep apnea?
It’s risky, but not impossible. If you have untreated sleep apnea, opioids can be deadly. However, if you’re using CPAP consistently and your apnea is well-controlled, your doctor may continue opioids at the lowest effective dose. Never combine opioids with alcohol, benzodiazepines, or other sedatives-this multiplies the risk.
Can I stop opioids to fix my sleep apnea?
Stopping opioids may improve breathing, but it’s not guaranteed. Some patients see significant improvement, while others still have apnea due to permanent changes in brainstem control. Never stop opioids cold turkey-withdrawal can be dangerous. Work with your doctor on a safe tapering plan while treating the sleep apnea with CPAP or other therapies.
Are there any new medications that treat pain without causing sleep apnea?
Researchers are testing drugs like cebranopadol, which targets pain receptors without strongly affecting breathing centers. These are still in clinical trials. For now, the safest approach is using the lowest effective opioid dose, combined with sleep apnea treatment. Non-opioid options like gabapentin, physical therapy, and cognitive behavioral therapy for pain should also be explored.
How often should I get tested for sleep apnea if I’m on long-term opioids?
Get tested before starting opioids if your dose will exceed 50 MEDD. After starting, repeat testing every 1-2 years-or sooner if you notice new symptoms like increased snoring, daytime sleepiness, or worsening fatigue. If your dose increases, get retested immediately. Sleep apnea can develop or worsen over time, even if you felt fine at first.

Comments (14)
Man, I had no idea opioids could mess with your breathing like this. My uncle’s been on methadone for years and just thought he was ‘sleeping too hard.’ Now I’m gonna send him this link. 😅
This is one of those topics that flies under the radar until it’s too late. I’ve seen friends on long-term pain meds who just ‘feel tired all the time’-no one connects it to breathing. But yeah, if you’re snoring like a chainsaw and waking up with a dry mouth, it’s not just bad sleep hygiene. It’s your brain forgetting how to breathe. 🤯
Thank you for sharing this. So many people are suffering silently, and this is exactly the kind of info that needs to be out there. Please, if you're on opioids and feel like you're always exhausted-get tested. It's not weakness. It's wisdom. 💙
Oh great. So now instead of just dying from addiction, we get to die from sleep apnea while on opioids? Brilliant public health move, America. 🙃
OMG I just realized my husband’s 100mg MEDD is probably why he snores like a freight train 😭 I’m booking a sleep study tomorrow. Also, acetazolamide?? Sounds like a wizard potion. 🧙♂️💊
Test for sleep apnea if on opioids. Simple. Do it.
Life is a balance, yes? Pain is real. Sleep is sacred. But when medicine steals your breath, we must ask: what are we healing for? We treat the body, but forget the soul that needs rest. This isn’t just medical-it’s spiritual. Wake up, not just your lungs, but your awareness.
Yeah, I’ve seen this in my clinic. Patients come in saying ‘I just can’t sleep well,’ and we blame stress. But then we run the sleep study and-boom-AHI of 42. And they’re on 80mg of oxycodone. It’s not coincidence. It’s pharmacology. Still, most docs won’t even ask. Sad.
Wait so if I’m on pain meds and I snore, I gotta get a machine? Can’t I just sleep on my side? I don’t wanna wear a mask. It’s weird.
Hey, I get it. CPAP feels like a space helmet at first. But I started one after my opiate-induced apnea diagnosis-and now I actually wake up feeling human. 😅 The mask? Yeah, it’s awkward. But not as awkward as your wife sleeping in the guest room because you’re snoring like a chainsaw. Worth it.
idk man i think this is all just big pharma scare tactics. i mean, i’ve been on vicodin for 10 years and i sleep like a baby. maybe i’m just lucky??
Of course this is happening. The FDA, CDC, and Big Pharma are in bed together-literally. They don’t want you to know that opioids cause apnea because then people would stop taking them and the opioid crisis would ‘collapse.’ But guess what? They’ve been hiding the truth since the 90s. The real reason they push CPAP? So you keep taking the drugs. They’re not trying to save you-they’re trying to monetize your sleep. I’ve read the leaked memos. They call it ‘respiratory dependency.’ It’s not a side effect. It’s a business model.
Interesting data, but the study sample sizes are questionable. Most of the cited research comes from tertiary care centers-highly selected populations. Generalizing to ‘100 million opioid users’ is statistically unsound. Also, the Nox T3 Pro has a 92% accuracy rate? Compared to what? Lab-grade polysomnography? That’s misleading. And acetazolamide? Off-label use without phase III trials is dangerous. Please be more precise.
So what you’re saying is… the government wants us to be tired so we don’t protest? This is mind control. They’re drugging us to keep us docile. Sleep apnea isn’t medical-it’s psychological warfare. They’re using opioids to suppress our breathing and our will. Wake up. This is the new normal. And they’re calling it ‘pain management.’