When you’re 75 or older, taking a pill isn’t just about following the label. Your kidneys don’t work the way they did at 30. That’s why kidney function matters more than ever when it comes to medication safety. Nearly one in three common prescriptions for seniors-like blood thinners, antibiotics, or pain meds-are cleared by the kidneys. If those kidneys are slowing down and no one checks, you risk toxicity, falls, confusion, or even hospitalization. This isn’t theoretical. It’s happening every day in homes and nursing facilities across the country.
Why Kidney Function Changes With Age
Your kidneys don’t suddenly fail as you age. They just get slower. By age 70, the average person loses about 35% of their kidney filtering capacity compared to their 20s. That’s because the tiny filters inside the kidneys-called nephrons-die off naturally. Blood flow to the kidneys drops. Muscle mass shrinks, which affects how creatinine (a waste product) builds up in the blood. All of this means standard lab numbers can lie.Here’s the problem: many doctors still rely on old formulas that assume your body is the same as a 40-year-old’s. But if you’re frail, thin, or have low muscle mass-common in older adults-your creatinine levels can look normal even when your kidneys are struggling. That’s why using the wrong formula can lead to dangerous overdoses.
The Equations That Actually Work for Seniors
There are four main ways to estimate kidney function. Only two are reliable for seniors.- Cockcroft-Gault (CG): This is the original formula, from 1976. It uses your age, weight, sex, and serum creatinine. But here’s the catch: if you use your actual body weight, it overestimates kidney function in obese people and underestimates it in those who are thin. The fix? Use ideal body weight instead. Studies show this cuts dosing errors by 25% in seniors.
- MDRD: Developed in 1999, this one was meant to be more accurate than CG. But it was designed for people with kidney disease-not healthy older adults. It underestimates kidney function in seniors without disease, leading to unnecessary dose reductions.
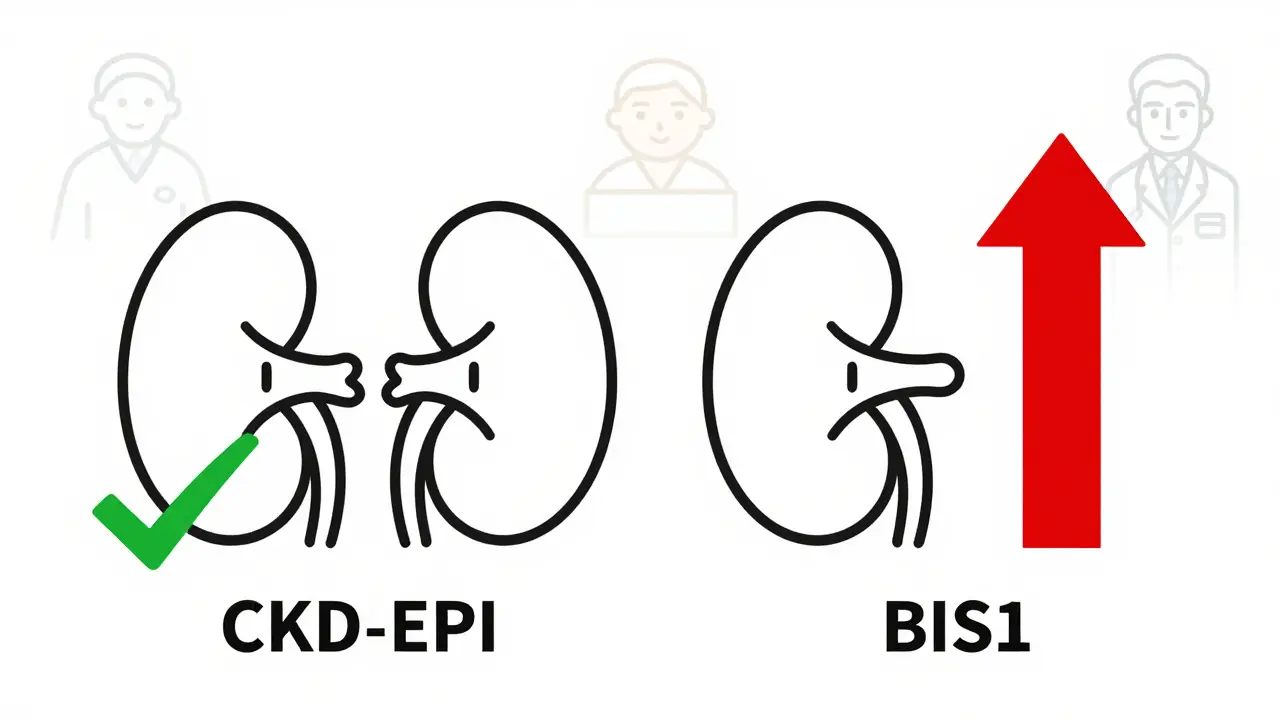
- CKD-EPI: Introduced in 2009, this became the new standard. It’s better than MDRD for most people, but it still struggles with very old adults, especially those with low muscle mass. It can misclassify someone with stage 3 kidney disease as stage 2, which might lead to a higher, unsafe dose.
- BIS1 and FAS: These are the new kids on the block. Developed specifically for older adults, they account for age-related muscle loss and frailty. BIS1, in particular, has been shown to be 15-20% more accurate than CKD-EPI in people over 80. One study found switching from CKD-EPI to BIS1 reduced medication-related hospitalizations by 18% in frail seniors.
So what should you use? For most seniors under 75, CKD-EPI is fine. But if you’re over 75, especially if you’re underweight, have dementia, or have multiple chronic conditions, BIS1 is the better choice. And if you’re obese or very muscular, CG with ideal body weight is still the gold standard.
What About Cystatin C?
Creatinine isn’t perfect. It’s made by muscle. So if you’ve lost muscle from aging, illness, or poor nutrition, your creatinine level drops-even if your kidneys are failing. That’s where cystatin C comes in. It’s a protein made by all cells, not just muscle. It’s not affected by body size or diet. A cystatin C-based eGFR is more accurate in frail seniors.The downside? It costs $50-$75 more than a standard creatinine test. Most insurance covers it, but many doctors don’t order it unless they’re suspicious of a mismatch. If your creatinine says your kidneys are okay, but you’re getting side effects from meds-ask for a cystatin C test. It’s a simple blood draw, and it can change everything.
What’s Not Reliable
Don’t trust any of these:- Using CG with actual body weight in thin or obese seniors
- Assuming eGFR from your EHR (electronic health record) is correct without checking which equation was used
- Using MDRD for healthy older adults
- Ignoring kidney function when prescribing drugs like warfarin, metformin, or gabapentin
One pharmacist in Melbourne told me about a 91-year-old woman on rivaroxaban (a blood thinner). Her EHR showed a CKD-EPI eGFR of 62. She was on the full dose. She started bleeding internally. A second test with BIS1 showed her true eGFR was 38. The dose was cut in half. She’s fine now. That’s not luck-that’s oversight.
How to Get It Right in Real Life
Here’s what works in practice:- Ask which equation your doctor uses. Don’t assume. Say: “Which formula did you use to calculate my kidney function?”
- Request BIS1 if you’re over 75. Especially if you’ve lost weight, eat poorly, or have trouble walking.
- Get cystatin C tested if your creatinine looks normal but you’re having side effects. It’s a red flag if your meds are making you dizzy or confused.
- Check your EHR settings. Some systems now auto-switch to BIS1 for patients over 75. If yours doesn’t, ask your doctor to manually override it.
- Keep a medication list. Bring it to every appointment. Highlight any drugs you’ve had side effects from. Include over-the-counter meds like ibuprofen or antacids-they hurt kidneys too.
Pharmacists are your allies here. Many senior care pharmacies now use BIS1 by default. If your pharmacist says, “We’re lowering your dose because your kidney function is lower than the EHR shows,” believe them.

What Happens If You Don’t Monitor
The risks aren’t small. In 2023, a national audit found that 30% of hospital admissions for seniors on kidney-cleared drugs were due to toxicity from incorrect dosing. That’s tens of thousands of preventable trips to the ER each year.Drugs like digoxin, lithium, and aminoglycosides have narrow safety margins. Even a 10% overdose can cause heart rhythm problems, seizures, or kidney failure. Metformin, a common diabetes drug, can cause lactic acidosis if kidneys aren’t working well. Gabapentin can cause falls and confusion. These aren’t rare side effects-they’re predictable outcomes of poor kidney monitoring.
What’s Changing in 2026
New tools are coming. In 2024, a new equation called CKD2024 was released. It combines creatinine and cystatin C with age-specific adjustments. Early results show it’s 15% more accurate in people over 80. The National Institute on Aging is funding a project to build point-of-care devices that estimate kidney function in under a minute-no lab needed.AI tools are also being tested. One prototype at Mayo Clinic looked at age, weight, muscle mass, diet, and meds to predict the best dosing formula. It cut errors by 22%. But until these tools are widely available, the best thing you can do is ask the right questions.
Bottom Line
Kidney function isn’t just a lab number. It’s your safety net for medication use as you age. Don’t let a default setting on a computer screen decide your dose. If you’re over 75, ask for BIS1. If you’re frail or losing weight, ask for cystatin C. If your doctor says, “Your kidneys are fine,” but you feel off after taking your meds-push back. Your kidneys are working harder than ever to keep you safe. The least you can do is make sure they’re being measured correctly.How often should seniors get their kidney function checked?
Seniors with no kidney disease or risk factors should have their kidney function checked at least once a year. If you have diabetes, high blood pressure, heart failure, or are taking multiple medications cleared by the kidneys, check every 3 to 6 months. Always check before starting a new medication or after a hospital stay.
Is a creatinine test enough for seniors?
Not always. Creatinine can be misleading in seniors because muscle mass declines with age. A normal creatinine level doesn’t mean normal kidney function. If you’re frail, underweight, or have lost appetite, ask for a cystatin C test. It’s more accurate for detecting true kidney decline in older adults.
Which formula should I ask for if I’m over 80?
Ask for the BIS1 equation. It was designed specifically for people over 75 and accounts for age-related muscle loss. Studies show it’s more accurate than CKD-EPI or Cockcroft-Gault in very old adults, especially those who are frail or malnourished.
Can I use an online eGFR calculator?
Yes-but make sure it lets you choose the formula. The National Kidney Foundation’s calculator (updated 2023) allows you to select BIS1, CKD-EPI, or Cockcroft-Gault. Never rely on an app or website that only uses one formula. Always verify which one your doctor used.
What if my doctor won’t use BIS1?
Bring printed guidelines from the American Geriatrics Society or the Journal of the American Society of Nephrology. Many doctors don’t know about BIS1. If they still refuse, ask for a referral to a geriatrician or nephrologist. Your safety matters more than institutional habits.
Are over-the-counter painkillers safe for seniors with reduced kidney function?
No. NSAIDs like ibuprofen and naproxen can cause sudden kidney injury in seniors-even if their eGFR looks okay. Acetaminophen (Tylenol) is safer, but don’t exceed 3,000 mg per day. Always check with your pharmacist before taking any OTC pain reliever.

Comments (9)
my grandma took ibuprofen for her arthritis and ended up in the ER last year. doc said her kidneys were fine but she was dizzy as hell. turns out they used CKD-EPI and she’s 82 with zero muscle. cystatin C test showed she was at 34. they cut her dose and now she’s walking again. why don’t more docs know this?
It is imperative to recognize that the physiological alterations inherent in the aging renal system necessitate a paradigmatic shift in pharmacokinetic evaluation. The reliance upon creatinine-based estimations constitutes a profound epistemological flaw in contemporary geriatric pharmacology.
Guys I just want to say this is the most important thing I’ve read all year. I’m a nurse in a nursing home and we’ve had three seniors hospitalized this year from blood thinners and gabapentin because the EHR just auto-filled CKD-EPI and no one checked. One lady started hallucinating after her dose didn’t change even though she lost 15 pounds in two months. We switched her to BIS1 and she’s back to recognizing her own kids. I printed out the guidelines and handed them to every doc on shift. If you’re over 75 and on meds - ask for BIS1. Don’t wait till you’re in the hospital. Your kidneys are working overtime just to keep you alive. The least you can do is make sure they’re being measured right. Seriously - do it today.
why do we even trust doctors anymore?? they just copy-paste from some dumb computer and call it medicine. my uncle died from lithium toxicity because his eGFR was ‘normal’ - turns out he had zero muscle and his cystatin C was off the charts. they didn’t even test it. now i make my mom bring her meds to the pharmacist before they’re filled. if your doc doesn’t know about BIS1? fire them. 🤬
I’ve been digging into this for months after my mom had a near-fatal reaction to metformin. The fact that CKD-EPI underestimates decline in frail seniors is wild - and it’s not even taught properly in med school. I reached out to the American Geriatrics Society and they sent me a 40-page white paper. The real problem isn’t the formulas - it’s the inertia. Hospitals still use EHRs that default to outdated equations. Even when you ask, they say ‘it’s what we’ve always done.’ But if you’re 80 and losing weight, ‘always’ is killing you. I’ve started a petition to make BIS1 the default for Medicare patients over 75. Anyone want to sign?
My dad’s pharmacist switched him to BIS1 last year after he dropped 12 lbs. Said the EHR was showing ‘mild’ kidney decline but BIS1 showed ‘moderate.’ They cut his gabapentin and his balance improved overnight. No drama, no yelling - just a quiet conversation with the pharmacist who actually read the guidelines. If you’re over 75, go talk to your pharmacist. They know more than your doctor sometimes. And yeah, cystatin C is worth the extra $60 if you’re feeling off after meds.
This is a Western medical fallacy. In India, we use clinical judgment, not equations. Creatinine is sufficient. These formulas are profit-driven tools for pharmaceutical corporations to justify more tests and more prescriptions. The elderly are being over-medicalized.
They’ve turned medicine into a spreadsheet. We used to trust doctors - now we’re supposed to argue with algorithms written by Ivy League grads who’ve never held a dying patient’s hand. This BIS1 nonsense? It’s another layer of bureaucracy to make us feel safe while the system keeps bleeding us dry. My grandfather died on warfarin because his lab numbers were ‘normal.’ They didn’t ask if he could walk to the bathroom. That’s what matters. Not equations. Not labs. Human observation.
THIS. IS. LIFE. OR DEATH. I’m a geriatric nurse practitioner and I’ve seen too many seniors get poisoned because their EHR auto-picked CKD-EPI and their doctor never questioned it. I now require BIS1 for every patient over 75 - and I demand cystatin C if they’re losing weight, confused, or dizzy. I’ve saved at least 12 lives this year just by asking two questions: ‘Which formula?’ and ‘Have you checked cystatin C?’ If your doctor resists - bring this post. Print it. Slide it across the table. You are not being difficult - you’re being smart. And if your pharmacist says ‘we’re lowering your dose’ - believe them. They’re the real heroes.