When you use an inhaler, you’re not just pressing a button and breathing in. If your technique is off, inhaler technique could be why your asthma or COPD isn’t improving-even if you’re taking your medicine exactly as prescribed. Studies show that 70 to 90% of people use their inhalers incorrectly. That means most of the medicine lands in your mouth or throat instead of your lungs, where it’s supposed to work. You might feel like the drug isn’t helping, but the real issue is how you’re using it.
Why Inhaler Technique Matters
Modern metered-dose inhalers (MDIs) deliver medication in tiny particles-50 to 150 microns wide. To reach deep into your airways, you need to breathe in slowly and steadily at about 30 liters per minute. If you inhale too fast, the particles hit the back of your throat and stick there. If you press the inhaler too early or too late, the mist floats away instead of being pulled into your lungs. The result? Only 10 to 20% of your dose actually gets to where it’s needed. That’s why you might still wheeze, cough, or need your rescue inhaler too often.
Medicine stuck in your mouth doesn’t just waste doses-it causes side effects. Inhaled steroids, like fluticasone or budesonide, can lead to oral thrush (a fungal infection) in 5 to 10% of users who don’t rinse their mouth after use. Worse, poor technique leads to more ER visits and hospitalizations. In the U.S. alone, improper inhaler use contributes to $1.5 billion in avoidable healthcare costs every year.
The 8-Step Correct Inhaler Technique
Follow these steps every time you use your MDI. Do them slowly. Don’t rush. Each step is designed to get the medicine where it belongs.
- Remove the cap and shake the inhaler. Shake it for 5 to 10 seconds-unless your inhaler is Alvesco or QVAR, which don’t need shaking. Shaking less than 5 seconds can reduce the dose by up to 40%.
- Breathe out fully. Exhale completely, as if you’re blowing out candles. Don’t exhale into the inhaler. Empty lungs make room for the medicine.
- Hold the inhaler correctly. Place the mouthpiece between your teeth and seal your lips tightly around it. Don’t hold it an inch away from your mouth-that’s an old trick for CFC inhalers. Modern HFA inhalers (like Ventolin HFA, Flovent HFA, or Symbicort) require a tight seal.
- Start breathing in slowly. As soon as you begin inhaling, press down on the inhaler to release the dose. Timing matters: inhale and actuate at the same time. Most people press too late-68% of errors are due to delayed actuation.
- Keep breathing in deeply and slowly. Aim for 3 to 5 seconds to inhale. You shouldn’t hear a whistling sound-that means you’re breathing too fast. Slow inhalation lets particles settle in your lungs.
- Hold your breath for 10 seconds. After inhaling, close your mouth and hold your breath as long as you comfortably can. Holding for 10 seconds increases lung deposition by 30% compared to breathing out right away.
- Breathe out slowly through your nose. Don’t blow hard. Let the air leave gently.
- Rinse your mouth with water and spit it out. Especially if you use a steroid inhaler. This cuts your risk of oral thrush by 40%. Don’t swallow the water.
Common Mistakes (And How to Fix Them)
Here are the five most common errors, based on data from the Pharmaceutical Journal and the American Lung Association:
- Not exhaling fully before inhaling. 42% of users skip this. Solution: Practice breathing out like you’re fogging up a mirror.
- Not holding breath long enough. 63% hold for less than 5 seconds. Solution: Count to 10 slowly in your head. Use your phone timer if needed.
- Inhaling too fast. 57% breathe in too sharply. Solution: Place a piece of paper in front of your mouth. If it moves, you’re inhaling too hard.
- Forgetting to prime the inhaler. 31% of users don’t prime new or unused inhalers. Solution: Spray 2 to 4 times into the air before first use or after two weeks of inactivity. Check your specific brand’s instructions-Alvesco needs 2 sprays, QVAR needs 4.
- Head tilted back or forward. 28% have poor head position. Solution: Keep your head straight, eyes forward. Tilted heads block airflow.
Spacers: A Game-Changer for Better Delivery
If you struggle with timing, a spacer (also called a valved holding chamber) can make a huge difference. It’s a tube that attaches to your inhaler. You spray the medicine into the spacer, then breathe in slowly from it. This removes the need to coordinate pressing and breathing.
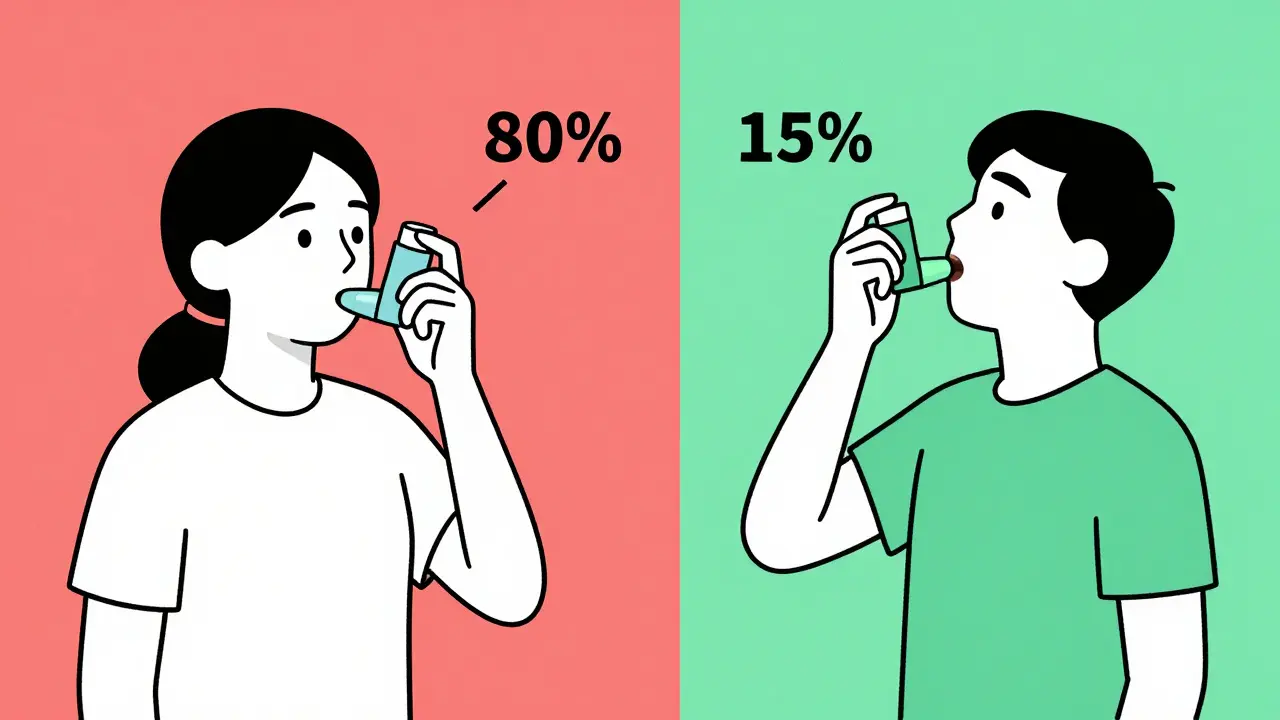
Spacers boost lung delivery from 10-20% to 70-80%. Patients using spacers have 45% fewer asthma attacks than those using MDIs alone. They’re especially helpful for children, older adults, and anyone with shaky hands or arthritis. For kids, use a spacer with a mask that fits snugly over the nose and mouth.
Don’t think spacers are just for kids. Many adults use them-and they’re just as effective. Clean your spacer weekly with warm water and let it air dry. Don’t wipe it with a towel-that creates static and traps medicine.
Smart Inhalers and New Tech
Technology is catching up to the problem. Smart inhalers now have built-in sensors that track when and how you use them. Apps like Propeller Health give real-time feedback on your technique, with 92% accuracy in detecting errors. These devices can alert you if you’re breathing too fast, forgetting to hold your breath, or missing doses.
By 2027, 25% of inhalers sold in the U.S. are expected to be smart models. The FDA now requires QR codes on all prescription inhalers by 2025, linking to official video tutorials. Some hospitals are even using virtual reality training-patients wear headsets to practice technique in a simulated environment. One Johns Hopkins study found VR improved long-term technique retention by 70%.

When to See Your Doctor
If you’ve been using your inhaler for months and still feel short of breath, it’s not just your condition-it’s likely your technique. Ask your doctor or pharmacist to watch you use your inhaler. Most won’t ask unless you bring it up. Don’t be embarrassed. Even nurses and doctors sometimes use inhalers wrong.
Bring your inhaler to your next appointment. Let them see the model, check the expiration date, and watch you go through the steps. If you use a spacer, bring that too. Many clinics now offer technique assessments as part of routine care. Since 2023, Medicare and Medicaid even reimburse providers $15 per assessment-so there’s an incentive for them to help.
Practice with a placebo inhaler if your doctor has one. These are empty devices that mimic the feel and weight of the real thing. Using them during training improves long-term retention by 65% compared to just being told how to do it.
Final Tip: Keep It Simple
You don’t need to memorize every detail. Just remember this: Shake, breathe out, seal, press as you breathe in, hold for 10, rinse. That’s it. Do those six things every time, and you’re doing better than 80% of users.
Improving your inhaler technique doesn’t mean changing your medication. It means getting the full benefit from what you’re already taking. Better technique means fewer symptoms, fewer pills, fewer hospital visits, and more days where you can breathe easy.
What happens if I don’t shake my inhaler before use?
Not shaking your inhaler can reduce the dose you get by 25 to 40%. The medicine and propellant inside can separate, so the first few puffs may contain mostly gas, not medication. Always shake for 5 to 10 seconds unless your inhaler is Alvesco or QVAR, which are designed not to require shaking.
Can I use my inhaler without a spacer?
Yes, you can-but only if you use perfect technique. Most people don’t. A spacer makes delivery more reliable by removing the need to coordinate pressing and breathing. It’s especially recommended for children, older adults, and anyone who finds timing difficult. Spacers can increase lung delivery from 10-20% to 70-80%.
Why do I get a sore throat after using my inhaler?
This is usually caused by steroid medication settling in your throat instead of reaching your lungs. Rinsing your mouth with water and spitting it out after every use cuts your risk of oral thrush and throat irritation by 40%. Don’t swallow the rinse-it can increase systemic side effects.
How do I know if my inhaler is empty?
Many inhalers have counters that show how many doses are left. If yours doesn’t, check the expiration date on the canister-it’s usually 12 to 24 months after first use. Don’t rely on how it feels or whether you hear a spray. Even empty inhalers can still make noise. When in doubt, replace it.
Is it okay to use an inhaler past its expiration date?
It’s not recommended. Medication can lose potency after expiration, and the propellant may not work as well. Even if the inhaler still sprays, you might not be getting the full dose. Always replace it by the date printed on the canister. For emergency rescue inhalers, never use an expired one.
Do I need to clean my inhaler?
Yes, especially the mouthpiece. Clean it once a week with warm water. Let it air dry completely-don’t wipe it with a towel. A clogged mouthpiece can block the medicine. Never use hot water or put it in the dishwasher.


Comments (8)
Been using my Flovent for years and never knew shaking it less than 5 seconds cuts the dose by 40%. That’s wild. I’ve been shaking it like I’m trying to cool off a soda.
so i just realized i’ve been pressing the inhaler after i start breathing in not at the same time… like 68% of people?? i’m not alone?? wow… also i never rinse my mouth… now i’m scared
Let me just say this: the entire medical-industrial complex has conditioned us to believe that inhalers are simple tools-when in reality, they’re precision instruments designed by engineers who clearly never met a human with asthma. The fact that you need a 10-second breath hold, perfect timing, and a spacer just to get 20% efficacy? That’s not a medical solution-it’s a systemic failure disguised as patient education. And don’t even get me started on the QR codes. Next they’ll be scanning your lungs.
There’s a deeper philosophical layer here that nobody’s talking about. The inhaler isn’t just a device-it’s a metaphor for modern healthcare. We’re given tools, instructions, and expectations, but no real support. We’re told to shake, breathe, hold, rinse-like if we just follow the steps, we’ll be cured. But what if the problem isn’t our technique? What if the problem is that we’re being asked to perform perfect bodily choreography while our bodies are falling apart? We’re not lazy. We’re exhausted. And yet the system keeps demanding more precision from people who are already gasping for air. The spacer isn’t a hack-it’s a plea for mercy. And the smart inhalers? They’re not helping us breathe better-they’re just logging our failures so insurers can raise premiums. We’re being surveilled while we struggle to inhale.
I’ve been using my inhaler wrong for 12 years. I thought the whistling meant it was working. Turns out it meant I was doing it wrong. I’m not mad. I’m just… disappointed. Like I was failed by the system. And now I have to relearn how to breathe.
I’ve been using my inhaler without rinsing for 8 years and never got thrush. So why should I trust this? Maybe it’s just fear-mongering to sell more mouthwash.
Just wanted to add: if you use a spacer, clean it weekly with warm water and air-dry it-never towel-dry. Static from towels traps medication and defeats the whole purpose. Also, for kids, make sure the mask seals fully around nose and mouth. My nephew went from 3 ER visits a year to zero after we got him a spacer with a proper mask. It’s not magic-it’s science. And it works.
Wait… so now they’re putting sensors in inhalers? And tracking when we use them? And linking to apps? And QR codes? And VR training? Who’s accessing this data? Is the government watching? Are insurance companies getting alerts when we miss a dose? What if I forget to use it during a panic attack? Will they cancel my coverage? I used to just need a puff. Now I need a PhD in inhaler engineering just to stay alive.