Switching from brand-name lithium to a generic version might seem like a simple cost-saving move-but for people with bipolar disorder, it can be anything but. Lithium carbonate is one of the oldest and most effective mood stabilizers ever developed, but its narrow therapeutic window means even small changes in how your body absorbs it can lead to serious consequences. When you switch between generic brands, your serum lithium levels can shift without you noticing-until you feel off, or worse, end up in the hospital.
Why Lithium Isn’t Like Other Medications
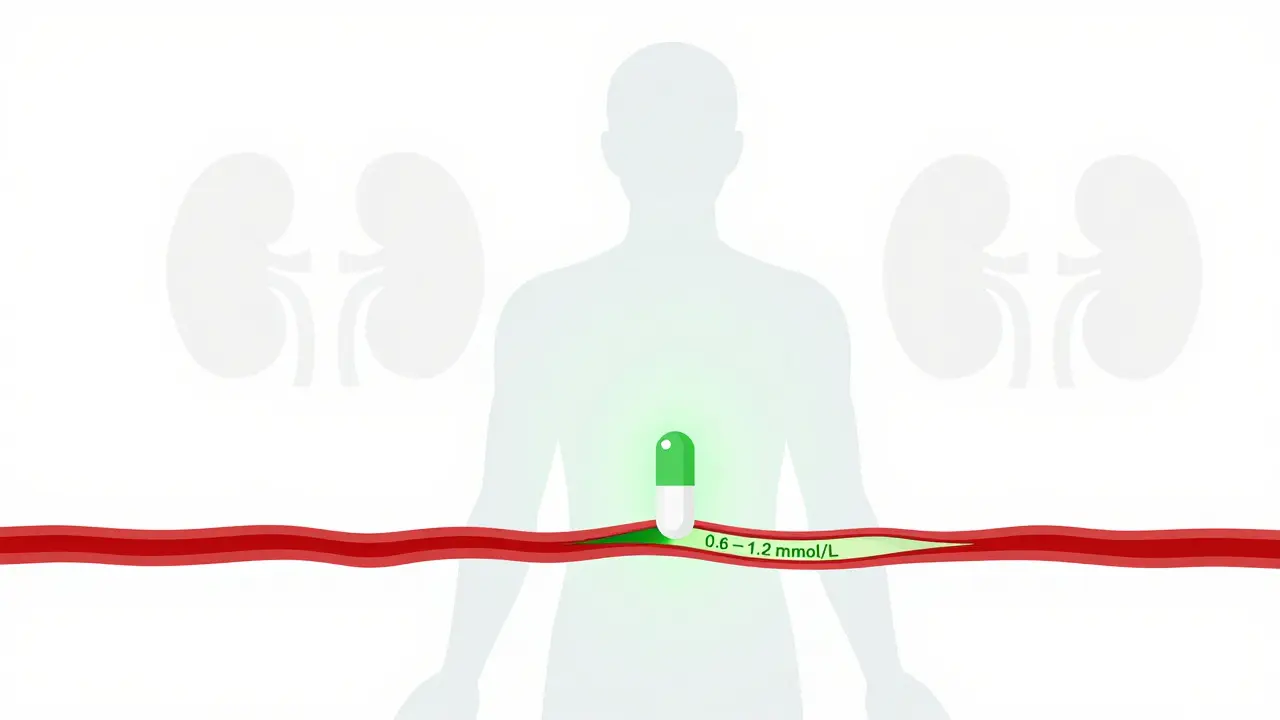
Lithium carbonate doesn’t work like antidepressants or antipsychotics. It’s not about how you feel on day one. It’s about keeping your blood level in a tiny window: between 0.6 and 1.2 mmol/L. Go below 0.6, and it stops working. Go above 1.5, and you risk toxicity-tremors, confusion, kidney damage, even seizures. The difference between healing and harm is less than a teaspoon of salt in a swimming pool.And here’s the catch: not all generic lithium carbonate pills are created equal. Even though the FDA requires generics to be "bioequivalent," that doesn’t mean they behave the same in your body. One brand might release lithium slowly over 8 hours. Another might dump it all into your system in 2 hours. That changes when your blood level peaks, how long it lasts, and whether you end up with too much or too little.
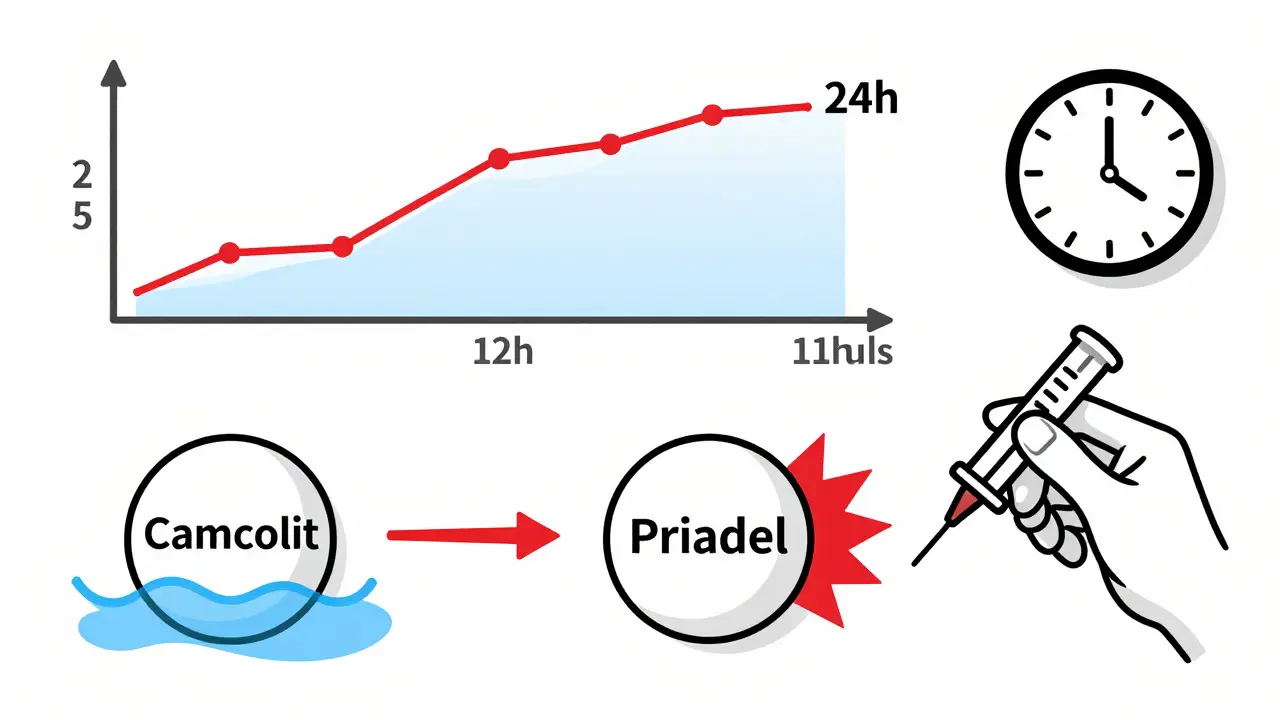
How Different Generics Affect Your Blood Levels
In 2024, a study in the Journal of Psychopharmacology tracked patients switched between two popular sustained-release generics: Camcolit and Priadel. Even when the daily dose stayed the same, those on Camcolit had, on average, 11% higher blood lithium levels. That’s not a fluke. Another study from decades ago found up to 20% variation in peak levels between two different sustained-release tablets with identical milligram labels.Why does this happen? It’s all about the coating, the granules, the release mechanism. One pill might dissolve slowly in your intestines. Another might break open faster. Your body doesn’t care about the name on the label-it cares about how much lithium enters your bloodstream and when.
Here’s what you need to know about common formulations:
- Immediate-release (e.g., Essential Pharma): Peaks in 2-3 hours. Requires 3 doses a day. Higher risk of spikes and side effects.
- Sustained-release (e.g., Priadel, Camcolit): Peaks in 4-5 hours. Often taken once or twice daily. Smoother levels, fewer side effects.
Switching from one to the other without adjusting your dose-or without checking your blood level-can be dangerous. A patient who’s stable on Priadel might suddenly hit 1.8 mmol/L after switching to a different brand, even if the doctor didn’t change the prescription.
What Your Doctor Should Be Monitoring
If you’re on lithium, your blood level should be checked regularly. But how often? And when? It’s not just about getting a test done.For immediate-release lithium, the blood draw should happen 12 hours after your last dose. For sustained-release? Wait 24 hours. That’s because the drug is still being released from the tablet. If you draw blood too soon, you’ll get a falsely high reading. Too late, and you’ll miss the peak. Both lead to wrong dose adjustments.
And it’s not just lithium levels. Your kidneys and thyroid need regular checks too. Lithium can slowly damage kidney function over years. It can also cause hypothyroidism in up to 15% of users. That’s why every 3-6 months, you need:
- Serum lithium level
- Estimated glomerular filtration rate (eGFR)
- Thyroid-stimulating hormone (TSH)
- Sodium and potassium
Some guidelines now recommend using cystatin C instead of creatinine alone to measure kidney function-it’s more accurate in older adults and those with low muscle mass.
Target Levels: Higher or Lower? The Debate
There’s no universal agreement on what the "right" lithium level is. Older studies, like the 1984 trial by Prien et al., showed that levels between 0.8-1.0 mmol/L cut relapse rates in half compared to 0.4-0.6 mmol/L. But newer guidelines, including the American Psychiatric Association’s 2021 update, suggest lower targets for maintenance: 0.6-0.8 mmol/L.Why the shift? Because we now know that even levels below 1.2 mmol/L can cause long-term kidney damage. And many patients feel better with lower doses. But here’s the twist: if you’re on a sustained-release formulation, you still need to aim for the higher end of that range-0.8-1.0 mmol/L-because the drug releases more slowly. Lower levels might mean it’s not working.
For older adults? Many experts recommend reducing targets by 20-25%. As we age, our kidneys clear lithium slower. A dose that was safe at 40 might be toxic at 70. A 2024 study found patients over 80 were taking, on average, 437 mg less lithium per day than those under 30-because their doctors knew to adjust.
When Switching Generics Is Risky
Pharmacists often substitute generics automatically. But lithium isn’t like statins or blood pressure pills. A switch from one brand to another-even if both are "generic"-can cause your levels to jump or drop without warning.One study documented four patients whose lithium levels spiked dangerously after a generic switch: readings of 1.32, 1.32, 1.88, and 1.35 mmol/L-all after a pharmacy substitution. One nearly had a seizure. Another ended up in the ER.
That’s why you need to:
- Ask your doctor to specify the brand on your prescription (e.g., "Dispense as written" or "Do not substitute").
- Get a blood test within 1-2 weeks after any switch.
- Report any new tremors, nausea, confusion, or frequent urination immediately.
Don’t assume your doctor knows what brand you’re on. Many don’t. And if your pharmacy switches it without telling you, you’re flying blind.
Who Should Avoid Lithium Altogether
Lithium isn’t for everyone. It’s dangerous if you have:- Severe kidney disease (eGFR under 30 mL/min)
- Brugada syndrome or other heart rhythm disorders
- Severe heart failure
- Dehydration or low sodium levels
Also, if you’re pregnant or planning to be, lithium carries risks to the developing heart. But it’s not an automatic no-many women take it safely with close monitoring. Talk to your psychiatrist and OB-GYN.

What’s Changing in Lithium Treatment
The future of lithium isn’t about new drugs-it’s about smarter dosing. Researchers are now looking at genetic markers that predict how fast your body clears lithium. The International Consortium on Lithium Genetics has found 30 genes linked to lithium response and clearance rates.Some hospitals are testing AI tools that use your age, weight, kidney function, and genetic data to predict your ideal dose before you even start. Imagine an app that tells your doctor: "Based on your profile, start at 600 mg of sustained-release lithium and check levels in 7 days."
But until that tech becomes standard, the rules stay simple: know your brand, know your level, and never skip a blood test.
Final Reality Check
Lithium is old, cheap, and underused-despite being one of the best tools we have to prevent suicide in bipolar disorder. Studies show it cuts suicide risk by up to 80% compared to other mood stabilizers. But its power comes with responsibility.Generic lithium saves money. But it doesn’t save lives if your blood level is off. If you’re on lithium, your health isn’t just about taking a pill. It’s about knowing your numbers, asking questions, and insisting on monitoring. No one else will do it for you.
Can I switch between lithium generics without checking my blood level?
No. Even if two generics have the same milligram strength, they can release lithium at different rates, causing your blood level to rise or fall unpredictably. Always get a serum lithium test 7-14 days after switching brands.
What’s the safest lithium level for long-term use?
For most adults on maintenance therapy, the safest and most effective range is 0.6-0.8 mmol/L. Higher levels (0.8-1.0 mmol/L) may be used during acute episodes, but long-term use above 1.0 mmol/L increases kidney and thyroid risks. Always follow your doctor’s personalized target.
Do I need to take lithium with food?
Lithium is best taken with food or right after meals to reduce stomach upset. But consistency matters more than timing. Take it the same way every day-always with food, or always on an empty stomach-to keep absorption stable.
Why do I need to drink so much water on lithium?
Lithium is cleared by your kidneys, and it competes with sodium. If you’re dehydrated or eat too little salt, your kidneys hold onto lithium, causing levels to rise dangerously. Drink 2-3 liters of water daily and avoid extreme low-salt diets. Don’t overdo it with diuretics or excessive caffeine.
Can I take other medications with lithium?
Many drugs interact with lithium. NSAIDs like ibuprofen, ACE inhibitors, and some antidepressants (especially SSRIs) can raise lithium levels and increase toxicity risk. Always tell every doctor you see that you’re on lithium. Even over-the-counter painkillers can be dangerous.
How often should I get my lithium level checked?
When starting or changing doses, check every 1-2 weeks. Once stable, check every 3-6 months. After any illness, dehydration, or medication change, check immediately. If you’re over 60 or have kidney issues, check every 2-3 months.
Are there alternatives to lithium if I can’t tolerate it?
Yes-valproate, lamotrigine, and quetiapine are common alternatives. But none match lithium’s ability to reduce suicide risk. If you can tolerate it, lithium remains the gold standard for long-term bipolar maintenance. Don’t give up on it without discussing the trade-offs with your psychiatrist.
What to Do Next
If you’re on lithium:- Find out exactly which brand you’re taking-write it down.
- Ask your pharmacist if your prescription was switched.
- Schedule your next blood test now, even if you feel fine.
- Keep a log of your mood, tremors, thirst, and urination frequency.
- Bring this information to your next appointment.
Staying stable on lithium isn’t about luck. It’s about knowing your numbers, knowing your brand, and never letting a pharmacy change it without your doctor’s say-so. Your brain depends on it.

Comments (15)
Lithium isn't just a pill-it's a tightrope walk. I've been on it for 12 years, and the only thing keeping me stable is knowing my exact brand and getting my levels checked every 3 months like clockwork. No exceptions. If your pharmacy swaps it without telling you, you're playing Russian roulette with your brain.
YES. THIS. I switched generics once-didn't think twice-and woke up with hands shaking like I'd had five espressos. Turned out my level was 1.7. ER. Two days. Now I have a sticky note on my pill bottle that says: 'DO NOT SUBSTITUTE.' My psychiatrist even wrote it on the script. Worth the extra $10.
The bioequivalence standard for lithium is fundamentally inadequate. The FDA's 80-125% AUC range permits clinically significant variability in sustained-release formulations. A 15% difference in peak concentration can push a patient from therapeutic to toxic. This is not a pharmacokinetic nuance-it is a systemic failure in regulatory oversight for high-risk medications.
As a psychiatrist in Mumbai, I've seen this exact scenario 17 times. Generic lithium substitution in India is rampant. Patients come in with tremors, polyuria, confusion-levels off the charts. We now mandate brand-specific prescriptions. No exceptions. And we check eGFR and TSH every 90 days, not 180. The cost of a lab test is pennies compared to a hospital admission.
They don't want you to know this-but big pharma loves lithium generics because they know people won't check their levels. They're counting on you to stay dumb. The FDA? They're in the pocket of the big labs. That's why they let brands like Camcolit and Priadel get away with 20% variation. It's not negligence-it's profit.
Interesting how the post ignores that most patients on lithium are elderly and on multiple meds. The real issue isn't the brand-it's polypharmacy. A patient on lithium, lisinopril, and ibuprofen for arthritis? That's a time bomb. No amount of brand consistency will save them if their doctor doesn't review their full med list.
I've been on lithium for 8 years. I take Priadel. I never switch. I get tested every 4 months. I drink water. I don't take Advil. It's not complicated. Maybe the problem isn't the drug-it's that we treat mental health like it's optional.
People don't understand that lithium isn't a medication-it's a lifestyle. It's not about feeling good. It's about surviving. I've lost friends to suicide because they stopped checking levels, thought they were fine, and then... gone. The fact that pharmacies can swap this without consent? It's a moral crisis. And nobody in power cares because bipolar disorder isn't sexy enough for headlines.
This is why Africa needs better meds-not more paperwork. In Nigeria, we don't even have consistent supply of brand-name lithium. Why are you worrying about Camcolit vs Priadel when most people can't get any? This post is for rich Americans who can afford to argue about generics. We're just trying to stay alive.
Too much text. Just say: Don't switch brands. Get tested. Drink water. Done.
Hey-I was terrified to start lithium. Thought it was for 'crazy people.' But once I found my dose and stuck with the same brand? I felt clearer than I had in years. If you're on it, don't let fear or laziness stop you from monitoring. You're not broken-you're managing something powerful. And you're not alone.
The British NHS has a similar issue. Generic lithium is routinely dispensed without brand specification. I have a patient who was switched twice in six months. Her TSH spiked, her creatinine rose, and she developed a tremor. We had to fight the pharmacy to reinstate the original brand. This is not a US-only problem-it is a global failure of medication safety protocols.
It's remarkable how such a simple molecule-lithium, the third element on the periodic table-holds such profound power over human emotion. We've used it for over 70 years, yet we still treat it like an afterthought. Perhaps the real question isn't about bioequivalence, but about how we value mental health in the first place. Is it a commodity? Or is it sacred?
I got switched to a new generic last month. Felt fine. Didn't check levels. Two weeks later, I was dizzy, nauseous, and couldn't focus. ER. Level: 1.8. Kidneys okay. But now I'm terrified to ever change anything. My doctor says I'm lucky I didn't seize. I'm not lucky-I'm just a statistic they don't care about.
ps. if ur dr says "its all the same" theyre wrong. and if ur pharmacist says "we substituted" without telling u? report them. this isnt just medical-its a civil rights issue for people with bipolar.