Medication Risk Checker for Hemolytic Anemia
Check Your Medication Risk
Enter any prescription, over-the-counter, or topical medication to determine if it poses a risk for hemolytic anemia.
Enter a medication name and click "Check Risk Level" to see if it poses a risk for hemolytic anemia.
When a medication turns your own body against you, it’s not just a side effect-it’s a medical emergency. Hemolytic anemia caused by drugs happens when your immune system or your body’s chemistry starts destroying red blood cells, sometimes within days of taking a pill. This isn’t common, but when it happens, it can drop your hemoglobin dangerously fast, leaving you breathless, pale, and at risk for heart failure. The key isn’t just knowing the symptoms-it’s recognizing which drugs can trigger this and acting before it’s too late.
How Medications Destroy Red Blood Cells
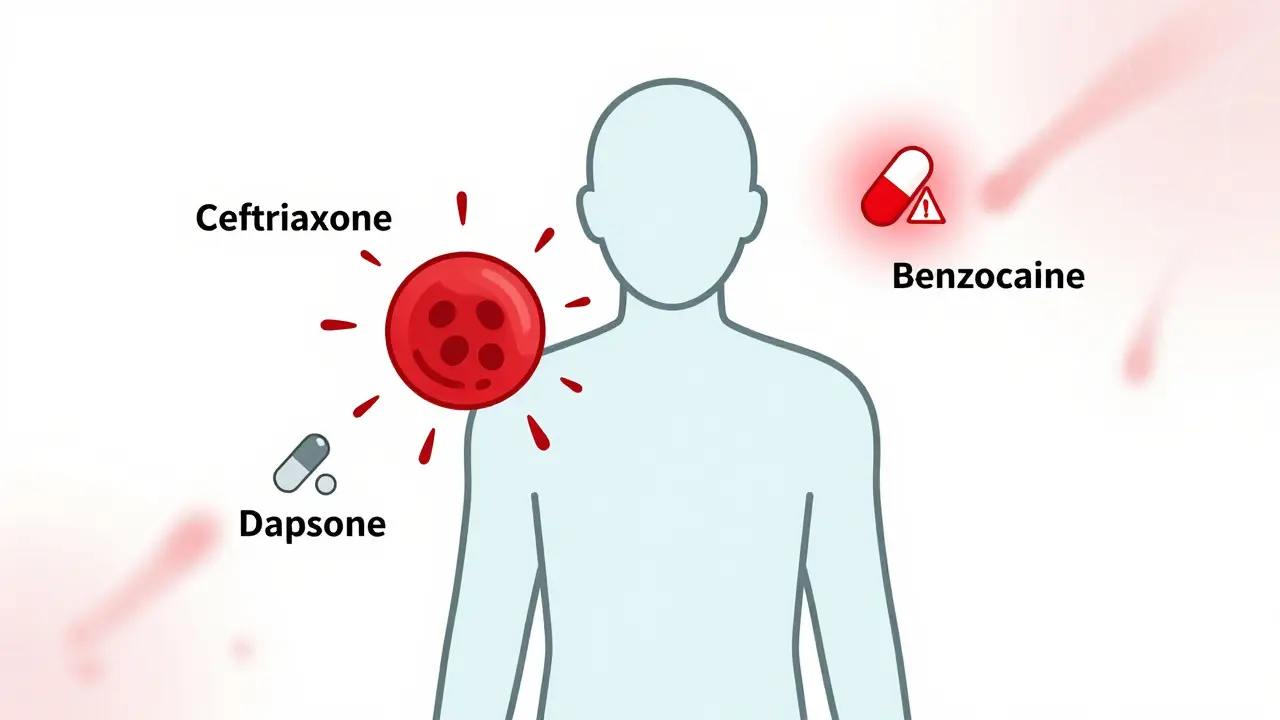
There are two main ways drugs cause red blood cells to break down. One is through the immune system; the other is through chemical damage. In immune-mediated cases, the drug binds to your red blood cells like a sticker. Your body sees this sticker as foreign and sends antibodies to attack. This is called drug-induced immune hemolytic anemia (DIIHA). The most common culprits? Cephalosporin antibiotics-especially cefotetan, ceftriaxone, and piperacillin. Together, these three make up about 70% of all immune-mediated cases. Methyldopa used to be a big offender too, but it’s rarely used now because doctors know the risk. The other way is oxidative hemolysis. Here, the drug doesn’t trigger antibodies-it directly damages the hemoglobin inside red blood cells. This happens mostly in people with G6PD deficiency, a genetic condition that affects about 1 in 10 African American men and up to 1 in 7 men in Mediterranean regions. But even if you don’t have G6PD deficiency, some drugs like dapsone, phenazopyridine, and nitrofurantoin can still cause oxidative damage. These drugs overload the cell’s ability to handle free radicals, leading to Heinz bodies-clumps of damaged hemoglobin that make red cells fragile and prone to bursting.Which Drugs Are the Biggest Risks?
You don’t need to avoid every medication, but you should know which ones carry the highest risk. The list is long, but the top offenders are clear:- Cephalosporins (cefotetan, ceftriaxone, cefoperazone)
- Penicillin derivatives (ampicillin, amoxicillin)
- NSAIDs (ibuprofen, naproxen-rare, but documented)
- Dapsone (used for leprosy and some skin conditions)
- Phenazopyridine (Pyridium, for urinary pain)
- Nitrofurantoin (a common UTI antibiotic)
- Levodopa (for Parkinson’s)
- Quinolones (levofloxacin, ciprofloxacin)
- Sulfa drugs and primaquine (especially dangerous if you have G6PD deficiency)
- Topical benzocaine (in numbing sprays and gels)
What’s important isn’t just the drug name-it’s the context. Someone with G6PD deficiency can have a severe reaction to a single dose of phenazopyridine. Someone without the deficiency might take it for weeks with no issue. That’s why a full medication history matters more than any single test.
What Does It Feel Like?
The symptoms don’t come out of nowhere. They build over days or weeks. Fatigue is the most common-reported in over 90% of cases. You feel tired even after sleeping. Then comes weakness, shortness of breath when climbing stairs, and a rapid heartbeat. Your skin may look pale or yellow. That yellowing? Jaundice. It’s not just a sign of liver trouble-it’s your body dumping bilirubin from all the broken-down red cells. In severe cases, hemoglobin can drop 3 to 5 grams per deciliter in just 72 hours. That’s like losing a third of your oxygen-carrying capacity overnight. Some people end up in the hospital with chest pain, irregular heart rhythms, or even heart failure. A 2022 review from the Cleveland Clinic found that 8% of patients with severe hemolytic anemia developed heart failure when hemoglobin fell below 6 g/dL.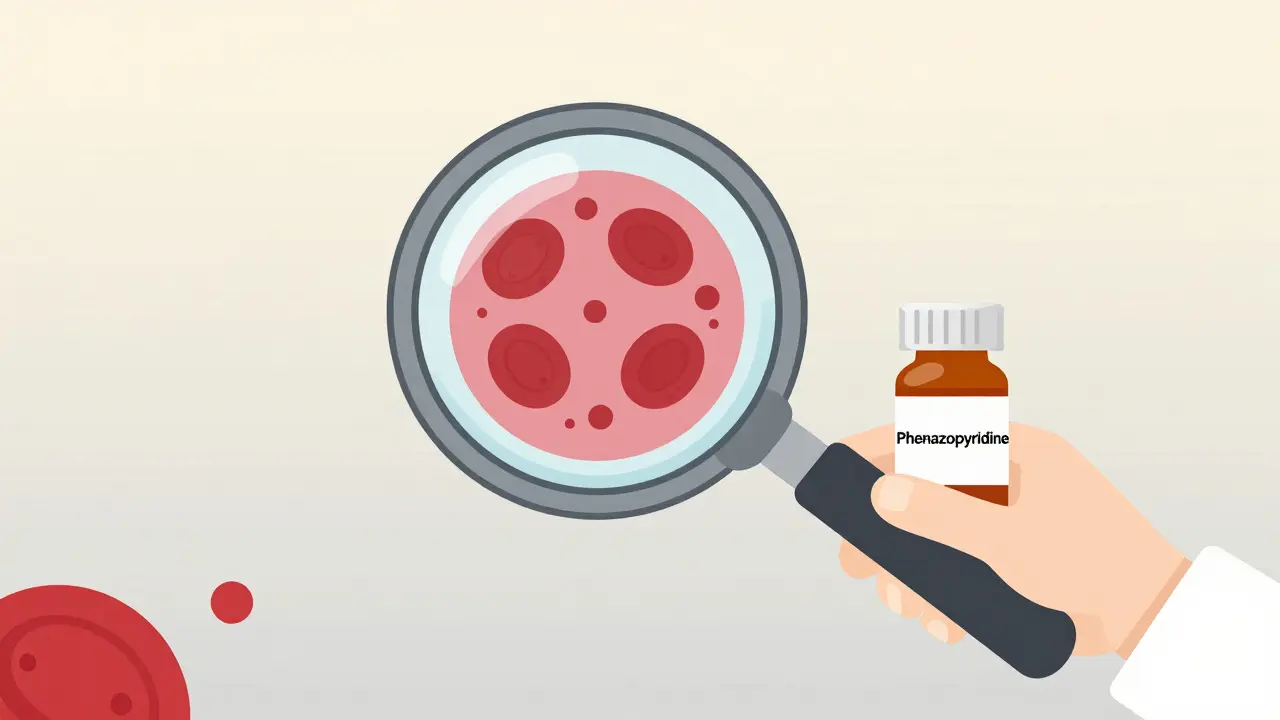
How Doctors Diagnose It
There’s no single test that says, “Yes, this drug caused it.” Diagnosis is a puzzle. Doctors start with three key blood markers:- Indirect bilirubin above 3 mg/dL
- LDH above 250 U/L
- Haptoglobin below 25 mg/dL
If these three are off, hemolysis is happening. Then comes the direct antiglobulin test (DAT)-also called the Coombs test. In immune-mediated cases, it’s positive in 95% of cases. But here’s the catch: if the drug is still in your system or if it’s a new reaction, the DAT can be negative. That’s why doctors don’t rule it out just because the test is negative.
For oxidative damage, they look at the blood smear. Heinz bodies-tiny dark clumps inside red cells-are a telltale sign. But they’re hard to see unless the lab knows to look for them. And if you have G6PD deficiency, testing for it during an active hemolytic episode can give false negatives. Why? Because the test measures enzyme levels in older red cells, and those are the ones getting destroyed. Newer cells still have normal G6PD, so the test looks fine. The real test should wait 2 to 3 months after recovery.
What Happens If You Don’t Stop the Drug?
The single most important thing you can do? Stop the drug. Immediately. No waiting. No second opinions. No “let’s see how it goes.” In 95% of cases, hemolysis stops within 7 to 10 days after removing the trigger. Hemoglobin levels begin to rise. Recovery usually takes 4 to 6 weeks. But if you keep taking it? The destruction continues. You can go from mildly anemic to critically ill in under a week. And here’s something many don’t realize: DIIHA puts you at higher risk for blood clots. Even though you’re losing red cells, your blood becomes stickier. One 2023 study found 34% of severe cases developed dangerous clots in veins-deep vein thrombosis or pulmonary embolism. That’s why doctors often give blood thinners even while treating the anemia.
Treatment: Beyond Just Stopping the Drug
Stopping the drug is step one. Step two? Supportive care. If your hemoglobin is below 7-8 g/dL, or if you’re dizzy, short of breath, or having chest pain-you’ll need a blood transfusion. But transfusions aren’t always simple. In immune-mediated cases, matching blood can be tricky because your body is making antibodies. The lab may need to do special cross-matching to find safe units. Corticosteroids like prednisone were once standard. But studies show they don’t speed up recovery much-unless your body keeps making antibodies even after the drug is gone. In those rare cases, doctors turn to stronger drugs: intravenous immunoglobulin (IVIG), then rituximab, azathioprine, or cyclosporine. About 78% of these refractory cases respond within 3 to 6 weeks. For oxidative hemolysis with methemoglobinemia (when iron in hemoglobin turns from ferrous to ferric), methylene blue is the fix. But here’s the danger: if you have G6PD deficiency, methylene blue can make things worse-by triggering more hemolysis. It’s absolutely off-limits in those patients.What You Can Do Now
If you’re on any of the high-risk drugs listed above and start feeling unusually tired, short of breath, or notice yellowing in your eyes, don’t wait. Talk to your doctor immediately. Bring your full medication list-even supplements and over-the-counter stuff. If you know you have G6PD deficiency, keep a printed list of unsafe drugs. Avoid phenazopyridine, sulfa drugs, and dapsone. Ask your pharmacist to flag any new prescription for potential oxidative risk. Hospitals are starting to use electronic alerts to warn doctors when someone on a high-risk drug shows early signs of anemia. One study showed this cut severe cases by 32% in 18 months. That’s progress. But it’s not perfect. You’re still your own best advocate.Why This Matters More Than You Think
Drug-induced hemolytic anemia is rare. But when it happens, it’s often missed. A 2024 study found that 43% of cases were misdiagnosed at first-mistaken for infections, liver problems, or even just “the flu.” Internal medicine residents correctly identified it in only 58% of cases on their first try. After training, that jumped to 89%. That’s the gap between a delayed diagnosis and a life saved. The good news? If caught early, recovery is nearly guaranteed. Most people bounce back fully. No long-term damage. No chronic illness. Just a reminder: your body can turn on a medication you thought was harmless. Listen to your symptoms. Know your risks. And never ignore sudden fatigue, jaundice, or rapid heartbeat after starting a new drug.Can you get hemolytic anemia from over-the-counter drugs?
Yes. While most cases are tied to prescription antibiotics or painkillers, even common OTC drugs like ibuprofen and naproxen have been linked to immune-mediated hemolytic anemia in rare cases. Topical benzocaine-found in numbing gels and sprays for teething or sore throats-has also caused oxidative hemolysis, especially in children. Always tell your doctor about everything you’re taking, even if you think it’s harmless.
Is hemolytic anemia from drugs more dangerous in older adults?
Older adults are at higher risk for complications, not because they’re more likely to develop it, but because their bodies handle stress less well. Heart and kidney function decline with age, so a sudden drop in hemoglobin can trigger arrhythmias or acute kidney injury faster than in younger people. Many seniors are on multiple medications, increasing the chance of a dangerous interaction. Monitoring hemoglobin levels after starting a new drug is especially important after age 65.
Can G6PD deficiency be tested before taking a risky drug?
Absolutely. If you’re of African, Mediterranean, or Southeast Asian descent, or have a family history of anemia after taking certain medications, ask for a G6PD test before starting drugs like dapsone, sulfonamides, or primaquine. The test is simple-a blood draw-and it’s covered by most insurance. If you’re deficient, your doctor can choose safer alternatives. Prevention beats emergency treatment every time.
How long does it take to recover from drug-induced hemolytic anemia?
Most people start to feel better within a week after stopping the drug. Hemoglobin levels typically begin rising by day 5-7 and return to normal in 4 to 6 weeks. Full recovery of red blood cell production takes longer-up to 8 weeks-because the bone marrow needs time to rebuild its supply. Fatigue may linger a bit longer, but it should gradually improve. If symptoms don’t improve after 10 days of stopping the drug, further testing is needed.
Are children at risk for drug-induced hemolytic anemia?
It’s rare in children, but when it happens, it’s often more severe. A 2023 study showed children with DIIHA had average hemoglobin levels of 5.2 g/dL-lower than the adult average of 6.8 g/dL. This means they’re more likely to need transfusions and experience heart strain. Newborns with G6PD deficiency are especially vulnerable to oxidative drugs like naphthalene (found in mothballs) or certain antibiotics. Always check with a pediatrician before giving any new medication to a child, especially if there’s a family history of anemia.

Comments (15)
Just had my doc slap me with ceftriaxone for a sinus infection last month. Felt like I got hit by a truck 3 days later-fatigue, yellow eyes, heart racing. I thought it was the flu. Turns out my haptoglobin was near zero. Glad I read this before I ignored it. Never taking cephalosporins again without asking first.
Also, side note: my pharmacist flagged it. That’s the kind of care we need more of.
The data presented lacks statistical context regarding incidence rates. While the clinical descriptions are accurate, the absence of population-at-risk denominators renders the perceived risk misleading. For instance, the incidence of DIIHA from ceftriaxone is approximately 1 in 10,000 exposures. Framing this as a common emergency is clinically irresponsible.
Yeah, I’ve seen this play out in the ER. Guy comes in with ‘flu symptoms’ after taking ibuprofen for a headache. Turns out he’s got a DAT-positive hemolytic anemia. He didn’t even know ibuprofen could do that. Honestly? Most people think ‘side effect’ means ‘mild stomach upset.’ This? This is your body eating itself.
And yeah, methylene blue is a trap for G6PD folks. Seen someone nearly die because the ER doc didn’t ask about ancestry.
so i had no idea any of this was a thing
i took nitrofurantoin for a UTI last year and felt like i was running on empty for weeks but i just thought i was tired from work
now im gonna ask my doc to test me for g6pd before any new med
thanks for the heads up, this couldve saved me a whole mess
This is so important for people in India too! Many take antibiotics without prescriptions, and G6PD deficiency is super common here. My uncle almost died from primaquine after a malaria episode. No one warned him. Please share this with your family, especially if you’re from South Asia. Prevention is everything.
Biggest issue I see? Doctors don’t ask about OTC meds. People think ‘just ibuprofen’ is harmless. But that’s what tripped up my cousin. She took it for a week with no problem, then got dizzy, turned yellow. Turned out her liver enzymes were fine, but her RBCs were getting shredded. She’s fine now, but she had to miss two months of work.
Always tell your doc about every pill, powder, or gel-even the ‘harmless’ ones.
wait so benzocaine in teething gel can do this??
my niece got that stuff last year and i thought it was just for numbing
now im scared to give her anything
also i think my grandpa had this and they just called it ‘anemia’ and gave him iron pills. he died 3 months later. maybe this was why
Let me get this straight-your body can literally turn a common antibiotic into a death sentence and you’re just supposed to ‘watch for fatigue’? That’s not medicine, that’s Russian roulette with a prescription pad.
And why aren’t these drugs labeled with a skull and crossbones? Why do we trust pharmaceutical companies to self-police? This is a systemic failure. Someone’s getting rich off people like me who almost died because no one told me to stop the damn drug.
lol so you’re telling me that if I take a painkiller and feel tired, I should panic? 😂
Next you’ll say aspirin causes spontaneous combustion. I’ve been on naproxen for 12 years. My RBCs are fine. Also, ‘heinz bodies’? Sounds like a band name. 🤓
Also, why is everyone so scared of antibiotics? I’ve got 3 kids and zero fear. Let ‘em get sick. Their immune systems need training. 🌈
so like… if i take tylenol and get tired, is that this? or just me being lazy?
also why do docs even give these drugs if they can kill you?
also why is this even a thing? why not just make safer pills?
also i think my cat has this. she’s always tired.
There’s something deeply human here. We treat meds like magic bullets, but our bodies aren’t machines-they’re ecosystems. When you introduce a foreign molecule, you’re not just treating a symptom-you’re stirring up ancient biological alarms.
That fatigue? It’s your red cells screaming. That jaundice? Your liver trying to clean up the mess. This isn’t just pharmacology-it’s a conversation between your body and a molecule it never asked for.
Listen to the whispers before they become screams.
It is imperative to underscore that the pathophysiological mechanisms delineated herein are predicated upon a robust clinical correlation between temporal drug exposure and hematologic derangement. The absence of prospective, randomized, controlled trials validating the causal inference in the majority of reported cases renders the current clinical paradigm speculative at best. One must exercise epistemological caution when generalizing from case reports to population-level risk assessments.
Wait… so you’re telling me Big Pharma knows this and still sells these drugs? 😳
And the FDA? They’re in on it. I bet they’re getting kickbacks from the labs that make the DAT tests. Why else would they let benzocaine be sold in baby teething gels?
Also, did you know that fluoride in water causes hemolysis? I read it on a blog. It’s all connected. You think this is about drugs? Nah. It’s about control. They want you tired so you don’t ask questions.
I’m so glad this got shared. My sister had this after taking dapsone for a rash. She thought it was just ‘bad allergies.’ Took her three weeks to get diagnosed. Now she’s fine, but she’s got a new rule: no new meds without a blood check first.
If you’re reading this and you’re on one of these drugs? Don’t wait. Talk to someone. You’ve got this. And if you’re scared? You’re not alone.
As an American woman, I find it unacceptable that foreign drugs like primaquine and sulfa are even allowed in our pharmacies. This is why we need border control for pharmaceuticals. These are third-world medications. We should be exporting our safe, American-made drugs to them-not importing their dangerous ones. This is a national security issue.