Topical Steroid Risk Assessment Tool
Assess Your Risk
This tool helps you understand your risk of skin atrophy and infections based on your topical steroid usage patterns. Results are not medical advice.
Enter your information to see your risk level
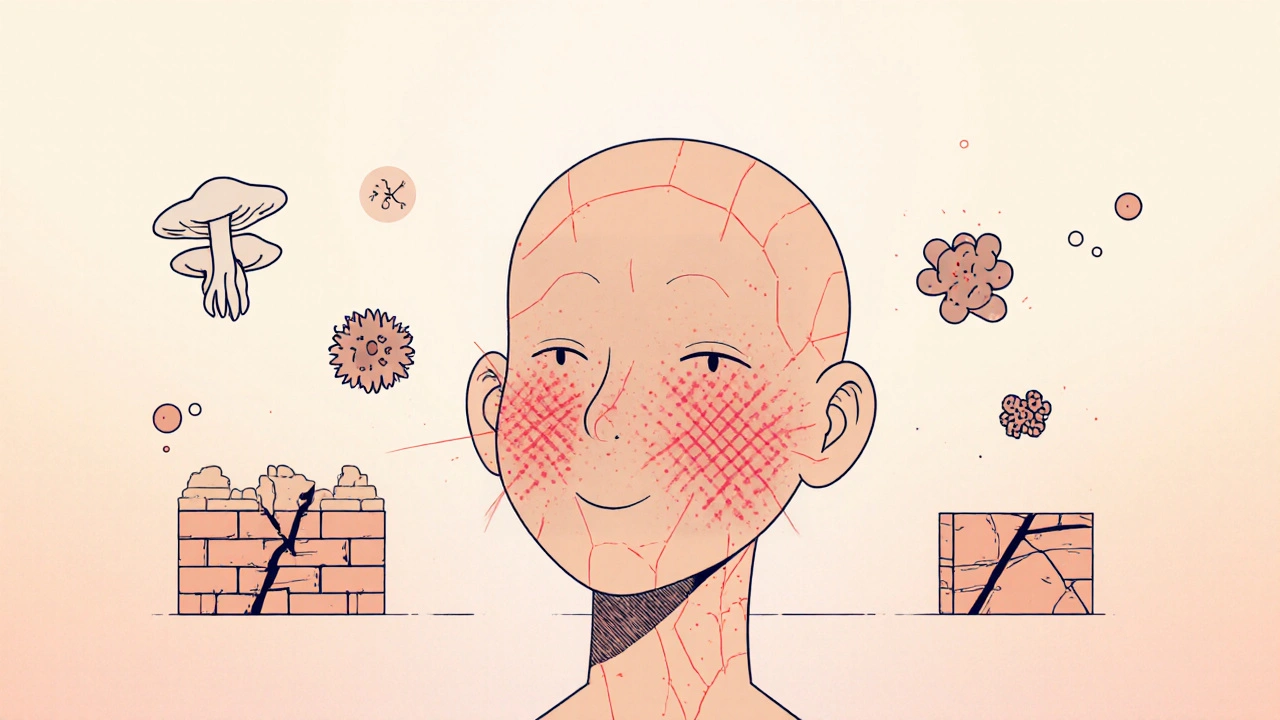
When you have eczema, psoriasis, or a stubborn rash, a topical corticosteroid cream can feel like a miracle. It calms the redness, stops the itching, and gives you back some peace. But what happens when that miracle starts to backfire? Over time, the very thing that helps can begin to break down your skin - thinning it, weakening its defenses, and opening the door to infections you never saw coming.
How Topical Steroids Start to Damage Your Skin
Topical corticosteroids work by shutting down inflammation. That’s good - until they shut down too much. These drugs don’t just target immune cells; they also interfere with the normal life cycle of your skin. Keratinocytes, the cells that make up the outer layer, slow down their production. Fibroblasts, the builders of collagen and elastin in the deeper layer, stop making the proteins that keep skin firm and resilient.
Research from 2006 and updated in 2025 shows that even short-term use - as little as three days - can begin to suppress collagen synthesis. The enzyme responsible for stabilizing collagen, prolyl hydroxylase, gets inhibited. Collagen mRNA, the blueprint for building this structural protein, starts breaking down. The result? Thinner skin. Less elasticity. A barrier that leaks moisture and lets in irritants and bacteria.
It’s not just about collagen. Your skin’s natural lipids - ceramides, cholesterol, and fatty acids - drop dramatically. These lipids form the mortar between the bricks of your skin cells. When they’re gone, your skin can’t hold water. Transepidermal water loss (TEWL) spikes. That’s why skin feels tight, flaky, and sensitive even when it doesn’t look inflamed.
What Skin Atrophy Actually Looks Like
Skin atrophy doesn’t always appear as obvious thinning right away. Early signs are subtle: your skin looks translucent, almost paper-thin. You might notice veins or capillaries becoming more visible - especially on the face or inner arms. These are telangiectasias, broken blood vessels that shouldn’t be there.
Over time, the skin loses its ability to bounce back. Wrinkles deepen in a unique way - not fine lines from aging, but deep, crinkled folds called "elephant wrinkles." These are hallmark signs of long-term steroid use and are often irreversible. Stretch marks (striae) may appear, even without weight gain. They start red or purple, then fade to silvery white. Once striae form, the damage is permanent.
Atrophy isn’t just cosmetic. It’s functional. Your skin’s barrier is compromised. That means it’s easier for bacteria like Staphylococcus aureus to invade, leading to infections. Fungal infections like candidiasis thrive in the warm, moist, immunosuppressed environment created by steroids. You might think it’s a flare-up of your original condition, but it’s not - it’s an infection hiding behind the redness.
Who’s at Highest Risk?
Not everyone who uses topical steroids gets atrophy. But some people are far more vulnerable.
- Potency matters: Class I-IV steroids (like clobetasol or betamethasone) carry the highest risk. Class V-VII (like hydrocortisone 1%) are much safer for long-term use.
- Location matters: The skin on your face, eyelids, neck, armpits, groin, and genitals is naturally thinner. These areas absorb steroids more easily and show damage faster.
- Duration matters: Using potent steroids for more than two weeks on sensitive areas increases risk dramatically. Daily use for months? That’s a recipe for atrophy.
- Age matters: Children’s skin is 3 to 5 times more absorbent than adults’. Their skin is still developing. Long-term steroid use in kids can stunt skin maturation and lead to permanent changes.
Studies show that about 17% of long-term users develop visible atrophy. Another 7% get striae. Around 6% develop rosacea or perioral dermatitis - conditions often misdiagnosed as eczema flare-ups.
Infections: The Hidden Consequence
When your skin barrier breaks down, infections follow. The most common are:
- Fungal infections: Candida albicans thrives under steroid creams. It looks like a red, scaly rash with tiny pustules around the edges - often mistaken for worsening eczema. It won’t improve with more steroid.
- Bacterial infections: Staph infections cause yellow crusting, oozing, and pain. They can turn into impetigo or cellulitis if untreated.
- Viral infections: Herpes simplex can flare into widespread, painful sores (eczema herpeticum) when steroids suppress local immunity. This is a medical emergency.
Many patients report that their rash gets worse after applying more steroid - not better. That’s a red flag. If your skin isn’t improving after 7-10 days, or if it’s getting more red, painful, or oozing, you’re likely dealing with an infection - not inflammation.
The Withdrawal Spiral: What Happens When You Stop
Stopping steroids after long-term use isn’t simple. Your skin has become dependent. The inflammation doesn’t vanish - it rebounds, often worse than before. This is known as Topical Steroid Withdrawal (TSW).
The pattern is predictable:
- Within a week of stopping, you get intense redness and burning - even if the skin looked fine before.
- After two weeks, peeling and flaking begin.
- Then comes a second flare: more redness, swelling, oozing.
- Each flare gets shorter, but the recovery periods get longer.
Patients in online communities report average recovery times of 8.2 months - some take over two years. The longer you used steroids, the longer withdrawal lasts. This isn’t just discomfort - it’s debilitating. People describe constant burning, sleep loss, and emotional distress. Many can’t wear makeup, go out in public, or work.

How to Prevent and Reverse the Damage
The best strategy is prevention.
- Use the weakest steroid that works. Start with hydrocortisone 1% unless your doctor advises otherwise.
- Apply only twice a day - never more.
- Limit use on the face, groin, or armpits to 5-7 days max.
- Never use steroid creams for more than 2-4 weeks without a break.
If you’ve already developed atrophy, stopping steroids is necessary - but it must be done carefully. Abruptly quitting potent steroids can trigger severe withdrawal. Work with a dermatologist to taper slowly: reduce frequency (from daily to every other day), then switch to a lower potency, then stop.
Barrier repair is key. Products with ceramides, cholesterol, and free fatty acids in a 3:1:1 ratio have been shown to restore 68% of barrier function in 8 weeks. Look for brands that list these exact ingredients in those proportions. Moisturize immediately after bathing, while skin is damp.
Sun exposure makes atrophy worse. UV rays break down collagen. Always use SPF 50+ broad-spectrum sunscreen on affected areas - even on cloudy days. Studies show it reduces collagen loss by 42%.
New Treatments on the Horizon
Scientists aren’t giving up on steroids - they’re trying to make them safer. New compounds called "dual-soft" glucocorticoid receptor agonists are being tested. These drugs aim to reduce inflammation without blocking collagen production. Early results are promising.
The NIH is running a Phase II trial (NCT04567892) on a topical formula that combines a low-dose steroid with fibroblast growth factor. This combo boosted collagen production by 63% compared to steroid alone over 12 weeks. It’s not available yet, but it’s a sign that safer options are coming.
Meanwhile, the global market for "steroid-sparing" treatments - like calcineurin inhibitors (tacrolimus, pimecrolimus) and PDE4 inhibitors (crisaborole) - is expected to grow from $1.2 billion in 2023 to $3.8 billion by 2028. More doctors are turning to these alternatives for long-term management.
What You Should Do Now
If you’ve been using a topical steroid for more than a few weeks:
- Check the potency. Is it a Class I-IV steroid? If yes, you’re at risk.
- Look for signs: thin skin, visible veins, stretch marks, persistent redness, burning without visible rash.
- Stop using it on sensitive areas unless directed by a doctor.
- Start using a ceramide-based moisturizer daily.
- Schedule a dermatology visit - don’t wait for symptoms to worsen.
Topical corticosteroids are powerful tools. But like any powerful tool, they need respect. Used wisely, they bring relief. Used carelessly, they can leave lasting damage. Your skin isn’t just a surface - it’s your body’s first line of defense. Protect it like one.
Can skin atrophy from topical steroids be reversed?
Early-stage skin atrophy - where the skin is thin but no stretch marks have formed - can improve over months after stopping steroids. Barrier repair creams, sun protection, and time can restore some thickness and function. But once striae (stretch marks) develop, the damage is permanent. The collagen structure is irreversibly broken. The goal then shifts to managing symptoms and preventing further damage.
How long does it take to recover from topical steroid withdrawal?
Recovery varies widely. Most people report symptoms lasting 6 to 18 months. Those who used potent steroids for less than a year often see improvement within 8-12 months. People using them daily for 5+ years may take 2-3 years or longer. The key is patience and consistent barrier repair. There’s no quick fix - but most people do recover fully with time and proper care.
Are over-the-counter hydrocortisone creams safe for long-term use?
Hydrocortisone 1% (OTC) is low potency and generally safe for short-term use - up to 2 weeks at a time. But using it daily for months, especially on the face or genitals, can still cause atrophy. The risk is lower than with stronger steroids, but it’s not zero. Always take breaks. If your rash returns after stopping, see a doctor - you may need a different treatment approach.
Can topical steroids cause infections even if I don’t see any signs?
Yes. Steroids suppress local immune responses, so infections can develop silently. A rash that doesn’t improve, gets worse, or becomes painful, oozing, or crusty is often infected - not inflamed. Fungal infections like candidiasis can look like a flare-up but won’t respond to more steroid. If you’re unsure, get it checked. A simple skin scraping can confirm if it’s yeast or bacteria.
What are the best alternatives to topical steroids for chronic skin conditions?
For eczema and psoriasis, non-steroid options include tacrolimus and pimecrolimus (calcineurin inhibitors), crisaborole (a PDE4 inhibitor), and dupilumab (an injectable biologic). These don’t cause skin thinning and can be used long-term. Barrier repair moisturizers with ceramides are also essential. Many patients use these alongside occasional short bursts of low-potency steroids - a strategy called "weekend therapy" - to reduce overall exposure.

Comments (10)
Just read this after my derm pulled me aside about my facial thinning. I was using clobetasol for 'eczema' for 8 months. Turns out it was just a fungal infection. The redness didn't go away because I kept layering steroid on top. Now I'm on tacrolimus and ceramide cream. Skin's slowly coming back. Don't be like me.
Y'all, I know how scary this sounds-but please don’t panic. I was in the same boat. Used hydrocortisone daily on my eyelids for 2 years thinking it was ‘just dry skin.’ Turns out I had steroid-induced rosacea. I cried for weeks. But guess what? After 14 months of barrier repair and zero steroids? My skin looks like skin again. Not perfect-but alive. You got this. 💪
Big Pharma made you dependent. 😏 They don’t want you to know about the 17% atrophy rate. That’s why they push ‘low-potency’ as ‘safe.’ Lol. It’s all a cash grab. I stopped cold turkey. Now I rub coconut oil on my face and pray to the sun gods. #SteroidFree
Really appreciate this breakdown. I’ve been using hydrocortisone 1% for my hands since 2021-twice a day, every day. Never thought twice about it. Now I’m cutting back to every other day and starting ceramide cream. Feels weird not reaching for the tube, but I’m trying. Anyone else doing the same? Also, what brand do you guys recommend? CeraVe? Eucerin?
As someone who grew up in a household where ‘itch = steroid cream’ was the only answer, this hit hard. My mom used clobetasol on my scalp for psoriasis from age 3 to 18. I have permanent striae on my neck. It took me 10 years to find a derm who even knew what TSW was. We need more awareness-especially in communities where doctors still treat skin like a ‘minor irritation.’ This post? Lifesaver.
Did you know… that prolyl hydroxylase inhibition… is directly linked to collagen mRNA degradation…? And that… the 3:1:1 ceramide ratio… is empirically proven… in multiple RCTs…? I’m not just saying this… I’ve read the papers… and cried… over my dermatology textbooks… at 3am… again…
I didn’t realize my ‘flare’ was actually a yeast infection until my derm scraped it. I thought I was being ‘bad’ with my skincare. Turns out, I was just suppressing my immune system. Now I use moisturizer like it’s oxygen. And I don’t touch the steroid tube unless it’s a full-on emergency. Game changer.
Topical corticosteroid-induced skin atrophy is a well-documented iatrogenic condition with prevalence estimates ranging from 10 to 20 percent in chronic users. Early intervention with barrier repair therapy and cessation of steroid use is critical. The data on ceramide-containing formulations is robust. I recommend initiating therapy immediately upon detection of translucency or telangiectasia. Delayed recognition leads to irreversible structural changes.
My kid was on hydrocortisone for eczema since 6 months old. We didn’t know it was too much until he was 4 and his inner elbows looked like parchment paper. We switched to pimecrolimus and now he’s 7 and his skin is healthy. No striae. No burning. Just soft. To all parents: don’t wait for the damage to show up. Ask your doctor about steroid-sparing options. Your child’s skin is still growing.
OH MY GOD I’M SO GLAD I READ THIS BEFORE I USED THAT CLOBETASOL ON MY NECK AGAIN. I THOUGHT I WAS BEING SMART-USING IT FOR ‘JUST A FEW DAYS.’ NOW I’M SCARED TO LOOK IN THE MIRROR. I’M GOING TO THE DERM TOMORROW. I’M NOT AFRAID ANYMORE. I’M READY TO HEAL. 🙏✨