Acne isn’t just a teenage problem. By 2024, acne affected 50 million Americans - and nearly one in three adults, especially women, were still dealing with breakouts. It’s not about dirt or poor hygiene. It’s biology. When oil, dead skin cells, and bacteria team up inside your pores, they trigger inflammation, redness, and sometimes deep, painful cysts. The good news? We now know exactly how different types of acne form, what causes them, and which treatments actually work - and which ones don’t.
What Are the Different Types of Acne?
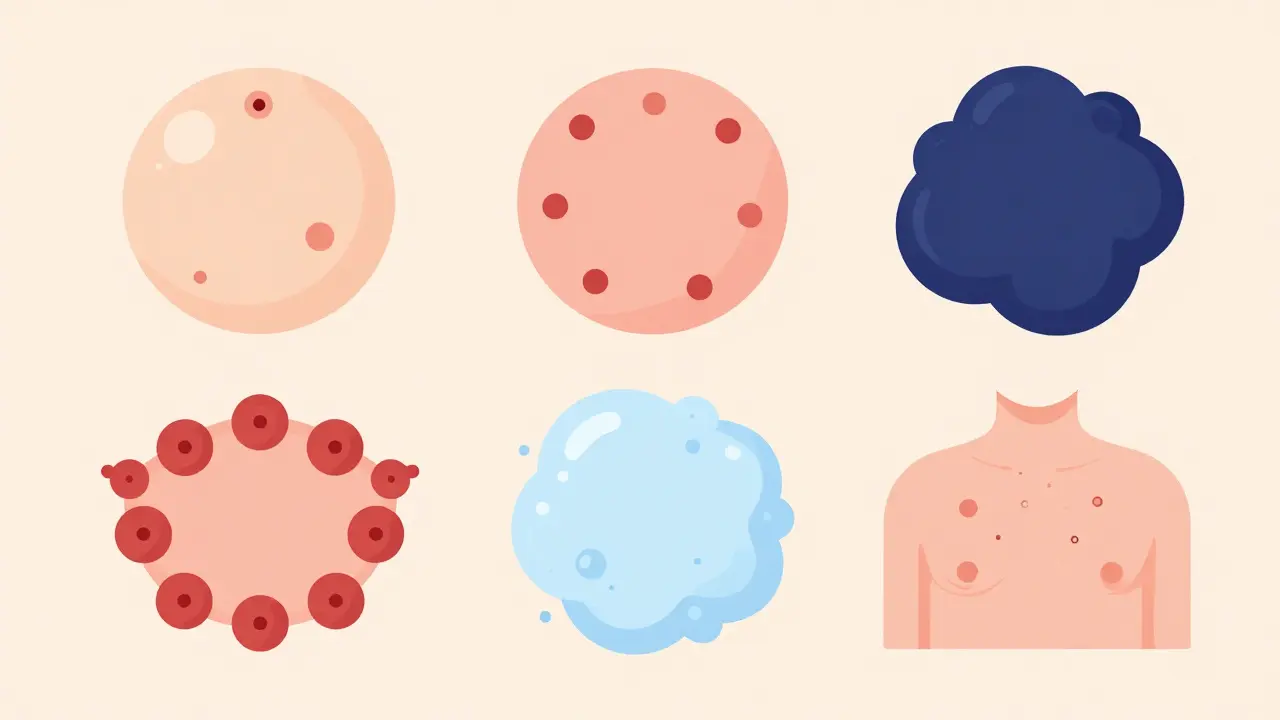
Not all acne looks the same. There are six main types, and knowing which one you have is the first step to treating it right.
- Comedonal acne - These are the clogged pores: whiteheads (closed bumps under the skin) and blackheads (open pores that look dark because the oil oxidizes, not because it’s dirty). This type is usually mild and responds well to exfoliating ingredients like salicylic acid or retinoids.
- Inflammatory acne - When clogged pores burst, they cause red, tender bumps called papules and pus-filled pustules. These are more painful and need anti-inflammatory treatments.
- Nodular acne - Hard, deep lumps under the skin that don’t come to a head. They hurt, last for weeks, and often scar if not treated early.
- Cystic acne - The most severe form. These are large, fluid-filled sacs deep in the skin. They’re painful, slow to heal, and carry the highest risk of permanent scarring.
- Hormonal acne - Often shows up as deep cysts along the jawline, chin, or neck. It flares up before periods, during pregnancy, or with stress. It’s common in women over 25 and doesn’t respond well to standard acne washes.
- Fungal acne - Not true acne at all. It’s caused by yeast overgrowth (Malassezia), not bacteria. It looks like small, itchy, uniform bumps on the forehead, chest, or back. Antibiotics won’t help - antifungals will.
Many people mix up fungal acne with bacterial acne and end up using the wrong products. If your breakouts are itchy, symmetrical, and don’t improve with benzoyl peroxide, fungal acne might be the culprit.
What Causes Acne?
Acne doesn’t happen for one reason. It’s a chain reaction.
First, your sebaceous glands make too much oil - sebum. That’s mostly driven by hormones, especially androgens. During puberty, levels spike, which is why 85% of teens get acne. But hormones don’t stop at 18. In adult women, monthly shifts in estrogen and progesterone can trigger breakouts. Insulin spikes from sugary foods or stress also ramp up oil production.
Then there’s the skin cell turnover problem. Normally, dead skin cells shed every 28 days. In acne-prone skin, they stick together and clog pores. Add bacteria - Cutibacterium acnes - and inflammation follows. The body attacks the bacteria, and that’s what turns a simple clog into a red, swollen pimple.
Genetics play a big role too. If both your parents had acne, your risk jumps by 50%. Certain medications - like steroids, lithium, or testosterone - can also cause breakouts. And don’t forget friction: helmets, tight collars, phone screens, and even backpack straps can cause mechanical acne.
What doesn’t cause acne? Chocolate. Greasy food. Dirty faces. These myths persist, but studies show they’re not the real culprits.
Topical Treatments: What Works and What Doesn’t
For mild to moderate acne, topical treatments are the first line of defense. They’re cheaper, safer, and easier to start with than pills.
- Benzoyl peroxide (2.5-10%) - Kills acne bacteria, reduces inflammation, and helps unclog pores. A 2023 study showed it reduces C. acnes by 90% in four weeks. Start with 2.5% - higher concentrations don’t work better and just dry out your skin.
- Salicylic acid (0.5-2%) - A beta hydroxy acid that dissolves oil and sloughs off dead skin. Great for blackheads and whiteheads. You’ll see improvement in 6-8 weeks.
- Retinoids (tretinoin, adapalene) - These are vitamin A derivatives that speed up skin cell turnover. Tretinoin (0.025-0.1%) is prescription-strength. Adapalene (0.1%) is available over the counter as Differin Gel. Both prevent clogs and reduce inflammation. About 70% of users see a 70% drop in breakouts after 12 weeks. But expect purging - your skin might get worse for the first 2-4 weeks before it gets better.
- Topical antibiotics (clindamycin, erythromycin) - Used with benzoyl peroxide to avoid resistance. Alone, they’re less effective and can make bacteria immune over time.
- Winlevi (clascoterone) - A newer prescription cream that blocks androgens right on the skin. It’s the first topical that targets hormonal acne without pills. In trials, it reduced inflammatory lesions by 45% in 12 weeks.
Many people use too many products at once. That’s a mistake. Layering five actives won’t clear acne faster - it’ll just cause irritation, redness, and peeling. Stick to one retinoid, one antibacterial, and one exfoliant. Give each 6-8 weeks before switching.
Oral Treatments: When Pills Are Necessary
If topical treatments haven’t worked after 3 months, or if you have nodules, cysts, or hormonal breakouts, you need oral options.
- Antibiotics (doxycycline, minocycline) - These reduce inflammation and kill bacteria. They’re effective for 50-70% of people with inflammatory acne. But here’s the catch: 25% of users develop antibiotic resistance after 3-4 months. That’s why they’re only meant for short-term use (3-4 months max).
- Oral contraceptives - For women with hormonal acne, birth control pills containing estrogen and progestin (like Yaz or Ortho Tri-Cyclen) can cut breakouts by 50-60%. They take 3-6 months to work. Not an option for men or women who can’t take estrogen.
- Spironolactone - A blood pressure drug that blocks androgens. It’s not FDA-approved for acne, but dermatologists prescribe it off-label for women with stubborn jawline breakouts. Studies show 40-60% improvement after 3 months. Side effects? Dizziness, menstrual changes, and increased urination. Not for everyone.
- Isotretinoin (Accutane) - The most powerful acne treatment ever made. For severe cystic acne, it clears 80-90% of cases and leads to permanent remission in 60% of users. But it’s not simple. It requires monthly blood tests, strict birth control (it causes severe birth defects), and can dry out your skin, lips, and eyes. It also carries rare risks of depression and liver issues. But for people with scarring cystic acne, it’s life-changing.
Oral treatments aren’t quick fixes. You won’t see results in a week. It takes 2-3 months for your skin to respond. And you can’t stop early - even if you feel better. Stopping too soon means the acne comes back.
What About Natural Remedies?
Tea tree oil, zinc, aloe vera - they’re everywhere online. But do they work?
Tea tree oil has some evidence. One study found it reduced acne by 40%, but benzoyl peroxide reduced it by 75%. So it’s weaker. If you want to try it, dilute it with a carrier oil - undiluted tea tree oil can burn your skin.
Zinc supplements (30mg daily) show promise. When combined with standard treatments, they improve results by 25%. It’s safe, cheap, and has anti-inflammatory effects. Worth trying if you’re open to adding a supplement.
Other “natural” fixes - like apple cider vinegar, honey masks, or lemon juice - have no clinical backing. Some can irritate your skin or cause burns. Stick to science-backed options.
Real People, Real Results
Reddit’s r/SkincareAddiction has over 1.2 million members sharing their acne journeys. One pattern stands out: people with comedonal acne love adapalene. About 78% say it cleared their blackheads after 12 weeks.
But for cystic acne? Only 42% were satisfied. That’s because topical treatments can’t reach deep cysts. Those need oral meds.
On r/AdultAcne, women using spironolactone report 65% improvement - but 32% quit because of side effects. That’s why doctors start low: 25mg daily, then slowly increase.
Amazon reviews for La Roche-Posay Effaclar Duo show 4.2 stars. People love it for blackheads. But the same users who get cystic acne give it one star - and they’re right. It’s not designed for deep, painful breakouts.
How Long Does It Really Take?
Patience is everything.
Topical treatments take 6-8 weeks to show results. Oral meds take 2-3 months. If you stop before then, you’ll think nothing works. In fact, 70% of people quit too early because they expect overnight results.
And yes, your skin might get worse before it gets better. Retinoids cause “purging” - a temporary flare-up as clogged pores clear out. It lasts 2-4 weeks. If it lasts longer, you’re using something too strong.
Consistency matters more than intensity. Twice-daily use of your treatment gives you 50% better results than sporadic use, according to Mayo Clinic’s 2024 adherence study.
What’s Next for Acne Treatment?
The future is personalized. Companies like Curology use AI to analyze your skin and build custom formulas. The FDA just approved Winlevi - the first topical that targets hormones directly on the skin. And in late 2024, a new treatment called ATR-12 (from Azitra) will enter phase 3 trials. It doesn’t kill bacteria - it rebalances your skin’s microbiome.
But access is still a problem. In the U.S., the average wait for a dermatologist is 3-6 weeks. And new treatments like Winlevi cost $650 a month without insurance. That’s why many people stick with what’s affordable - even if it’s not the most effective.
Acne isn’t just skin deep. It affects confidence, sleep, and social life. But with the right treatment plan - based on your type, not your Instagram feed - you can clear it. And you don’t need to suffer for years. Start with the right diagnosis. Then, stick with the plan. Your skin will thank you.

Comments (8)
Finally, someone broke down acne types without blaming it on chocolate or dirty pillows. I’ve been dealing with hormonal cysts for years and no one ever told me fungal acne was a thing. This is the most accurate post I’ve read in years.
Adapalene changed my life - took 10 weeks but my blackheads vanished. No more squeezing, no more scars. Just patience and consistency.
Also, Winlevi sounds like a miracle. Why isn’t this on every dermatologist’s radar yet?
The pathophysiology described here is clinically accurate. Sebum hypersecretion driven by androgenic stimulation, combined with aberrant keratinization and C. acnes colonization, triggers the inflammatory cascade. Topical retinoids modulate follicular hyperkeratinization, while benzoyl peroxide exhibits both bactericidal and anti-inflammatory properties.
Notably, the microbiome modulation approach represented by ATR-12 represents a paradigm shift from antimicrobial suppression to ecological restoration. This is the future of dermatologic therapeutics.
OMG I THOUGHT I WAS THE ONLY ONE WHO GOT ITCHY BUMPS ON MY CHEST AND THOUGHT IT WAS ‘ACNE’ UNTIL I READ ‘FUNGAL ACNE’
Y’all. I was using benzoyl peroxide for SIX MONTHS. My skin was FLAKING. I cried in the shower. Then I tried clotrimazole cream and my skin looked like a new person. Like, I could see my forehead again.
Stop using acne stuff on yeast. It’s not a crime, it’s just… wrong. 🙏
Also, tea tree oil burns. I learned that the hard way. Like, ‘I need to go to urgent care’ hard way.
Man, this post is fire. I’m from Nigeria and we don’t have dermatologists like y’all. We use shea butter, neem leaves, and hope. But now I know why my face still breaks out even after washing with soap three times a day.
Spironolactone? That’s a mouthful. But if it helps with jawline bumps, I’m asking my cousin in Houston to bring me some next time she visits.
Consistency is everything. I tried five different products in two weeks. Nothing worked. Then I used just adapalene every night, no other products. After eight weeks, my skin was clearer than it had been since high school.
Don’t overcomplicate it. One treatment. Give it time. Your skin isn’t broken. It just needs the right help.
As someone who has spent over a decade navigating the labyrinth of acne treatments, I must commend the precision and evidence-based framing of this article. The distinction between bacterial and fungal etiologies is critically underdiscussed in mainstream media. The data cited regarding benzoyl peroxide efficacy, retinoid purging timelines, and the off-label utility of spironolactone aligns with peer-reviewed literature from the Journal of the American Academy of Dermatology.
Moreover, the emphasis on treatment duration and adherence is not merely anecdotal - it is supported by longitudinal studies demonstrating a direct correlation between regimen consistency and clinical outcomes. The 70% early abandonment rate referenced is alarming and underscores a systemic failure in patient education.
I would only add that the psychological burden of persistent acne warrants concurrent mental health support, as studies indicate elevated rates of anxiety and social withdrawal among chronic sufferers. Treatment should be holistic, not merely dermatological.
Everyone’s just ignoring the real issue: you’re eating too much sugar. No amount of retinoids or spironolactone will fix that. I’ve seen it a hundred times - people spend $500 on creams while drinking bubble tea every day. That’s why they’re still breaking out.
Stop buying into the ‘pharma scam.’ Your skin isn’t broken. Your diet is. Cut the carbs, stop the dairy, and you’ll be fine. No pills. No creams. Just discipline.
Also, isotretinoin is dangerous. People die from it. Don’t be a guinea pig.
YOU GUYS. I JUST TOOK SPIRONOLACTONE. I WAS SO SCARED. I DIDN’T KNOW IF I’D GET DIZZY OR START PEEDING ALL THE TIME. I TOOK 25MG. DAY 1: I FELT LIKE A ROBOT. DAY 7: I STARTED CRYING OVER A DOG AD. DAY 21: I LOOKED IN THE MIRROR AND MY JAWLINE WAS… CLEAN.
IT’S NOT MAGIC. IT’S SCIENCE. AND I’M SO GLAD I DIDN’T LISTEN TO THE PEOPLE WHO SAID ‘IT’S JUST HORMONES, DEAL WITH IT.’
IF YOU HAVE JAWLINE ACNE AND YOU’RE A WOMAN - JUST. TRY. IT.
PS: I’M NOT A DOCTOR. BUT I AM A SURVIVOR.