Anticholinergic Burden Calculator
The Anticholinergic Cognitive Burden (ACB) scale measures how much a medication affects brain function. Medications with higher ACB scores increase risk of confusion, memory problems, falls, and dementia, especially in older adults. Calculate your total ACB score to understand your risk.
Select Medications
Selected Medications
Combining antihistamines with other sedating drugs can be dangerous - and many people don’t realize it until it’s too late. You might take Benadryl for allergies, then grab a sleep aid, or maybe you’re on anxiety medication and think a little diphenhydramine won’t hurt. But when these drugs mix, your brain slows down more than you expect. The result? Extreme drowsiness, confusion, slowed breathing, even hospital visits. This isn’t theoretical. It’s happening every day, especially in older adults and people taking multiple prescriptions.
Why First-Generation Antihistamines Are Risky
Not all antihistamines are the same. The ones you find over-the-counter - like diphenhydramine (Benadryl), hydroxyzine, and promethazine - are first-generation. They were designed decades ago to block histamine and relieve sneezing, itching, and runny nose. But they also cross the blood-brain barrier easily. That’s why they make you sleepy. And that’s exactly what makes them dangerous when paired with other sedating drugs.These medications don’t just cause drowsiness. They have strong anticholinergic effects, meaning they block acetylcholine, a key brain chemical involved in memory, attention, and muscle control. On the Anticholinergic Cognitive Burden (ACB) scale, diphenhydramine scores a 3 - the highest level. That’s worse than many prescription sedatives. When you add it to a benzodiazepine like Xanax or a painkiller like oxycodone, the effect isn’t just added - it’s multiplied.
Studies show that combining diphenhydramine with lorazepam increases sedation by up to 37% in cognitive tests. In real life, that means someone might fall asleep behind the wheel, stumble and fracture a hip, or stop breathing while sleeping. The CDC reports that when opioids and first-gen antihistamines are taken together, the risk of respiratory depression jumps from 1.5% to nearly 9%.
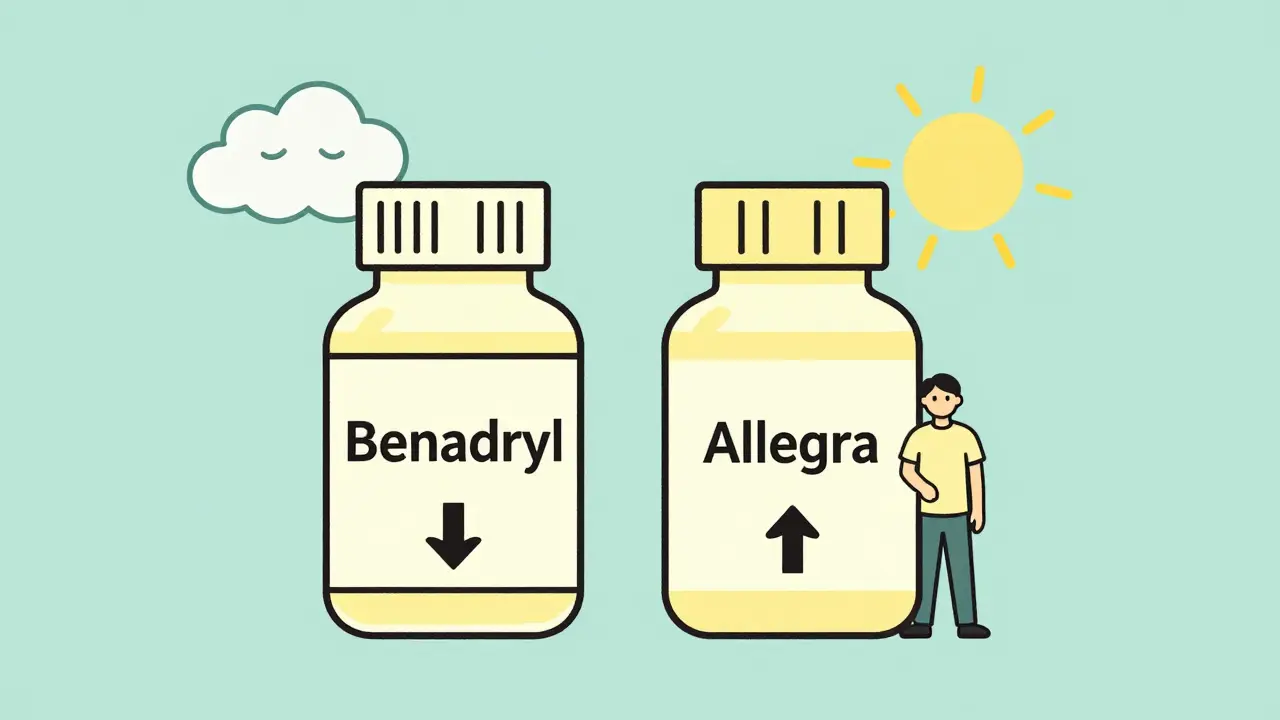
Second-Generation Antihistamines Are Safer - But Not Perfect
If you’re looking for allergy relief without the drowsiness, second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are the way to go. These were developed specifically to avoid the brain. Thanks to special transporters in the blood-brain barrier, they stay mostly outside the CNS. That’s why most people taking them report no drowsiness - 97% in one survey said they felt alert.They also score much lower on the ACB scale: 0 or 1. That means less risk of confusion, memory problems, or urinary retention - especially important for older adults. But don’t assume they’re risk-free. Cetirizine still has a score of 1, and if you’re taking multiple drugs that depress the central nervous system - like sleep pills, muscle relaxants, or even some antidepressants - even a low-score antihistamine can tip the balance.
Recent research on bilastine, a newer second-gen antihistamine, shows no interaction with lorazepam even at high doses. This points to a future where antihistamines won’t interfere with other meds at all. But for now, stick with the proven options: loratadine and fexofenadine are your safest bets.
What Medications Should You Avoid Mixing?
Here’s what you need to watch out for - and it’s more than just alcohol or sleeping pills:- Benzodiazepines: Xanax, Valium, Ativan - these are prescribed for anxiety and insomnia. Mixing them with diphenhydramine can cause extreme sedation, memory loss, or respiratory failure.
- Opioids: Oxycodone, hydrocodone, codeine - even low doses become risky with first-gen antihistamines. The CDC found 8.7% of people on this combo had serious breathing issues.
- Sleep aids: ZzzQuil, Unisom, and many generic sleep medications contain diphenhydramine or doxylamine. Taking them with another sedative is like double-dosing.
- Alcohol: One drink with 25mg of Benadryl can cause blackouts. Users on Reddit and WebMD report hospital visits after just one cocktail.
- Antidepressants: Some SSRIs and tricyclics have anticholinergic properties. Add them to diphenhydramine and you’re stacking risk.
- Antipsychotics and muscle relaxants: These also slow brain activity. Combined, they can lead to delirium, especially in seniors.
Even cimetidine (Tagamet), a common heartburn drug, is a problem. It blocks liver enzymes that break down antihistamines, causing them to build up in your blood. That means even a normal dose of Benadryl can become toxic if you’re also taking Tagamet.
Why Older Adults Are at Highest Risk
If you’re over 65, your body doesn’t clear these drugs the way it used to. First-gen antihistamines like diphenhydramine are cleared 50-70% slower in older adults. That means even a single dose lingers longer, increasing side effects. The American Geriatrics Society added diphenhydramine and hydroxyzine to its Beers Criteria - a list of medications that should be avoided in seniors because they cause more harm than benefit.One 2021 JAMA study found that when older adults took diphenhydramine with other anticholinergic drugs - like oxybutynin for overactive bladder - their risk of delirium jumped by 54%. Another study linked long-term use of these drugs to a 54% higher risk of dementia over 10 years.
Many seniors take multiple meds. The average Medicare patient is on nearly 8 prescriptions. Add OTC antihistamines for allergies or sleep, and you’re looking at a dangerous cocktail. Doctors often miss these combinations because patients don’t mention OTC drugs. That’s why it’s critical to bring your entire pill bottle - including vitamins and supplements - to every appointment.
Real Stories, Real Consequences
You don’t need to guess whether this is serious. People have lived through it.On Reddit, a user posted: “Benadryl + Xanax nearly killed me.” They took 50mg of diphenhydramine with 1mg of alprazolam and woke up in the ER with dangerously low breathing. The thread had 478 upvotes and 87 similar stories.
WebMD users report that 41% of those taking diphenhydramine with opioids experienced severe dizziness requiring medical help. BuzzRx documented over 1,200 reports of people blacking out after combining Benadryl with just one drink of alcohol.
Meanwhile, Allegra (fexofenadine) has a 4.3/5 rating on Amazon with over 18,000 reviews - most praising “no drowsiness even with my other meds.” Benadryl? Only 2.9/5, with 68% of negative reviews citing “dangerous interactions.”
What You Should Do Instead
Here’s how to stay safe:- Switch to second-gen antihistamines. Use loratadine, fexofenadine, or bilastine for allergies. They work just as well without the brain fog.
- Check your ACB score. Use the University of Washington’s free Anticholinergic Burden Calculator. Add up the scores of all your meds - including OTC. If your total is 3 or higher, talk to your doctor about deprescribing.
- Never use diphenhydramine as a sleep aid. It’s not safe long-term, and it’s not effective beyond a few nights. Try melatonin or cognitive behavioral therapy for insomnia instead.
- Tell every doctor you see - including pharmacists - about every pill you take. This includes herbal supplements, alcohol, and OTC drugs.
- Ask about alternatives. If you’re on oxybutynin for bladder issues, ask if tolterodine or mirabegron is an option - both have lower anticholinergic scores.
Pharmacies are now required to put bold warnings on diphenhydramine packaging: “May cause severe drowsiness when combined with alcohol, opioids, or sleep medications.” But many people still miss it. Don’t rely on labels. Ask questions.
What’s Changing in 2026
The tide is turning. Since 2018, sales of first-gen antihistamines have dropped 12.7% each year. Second-gen now make up 83% of the OTC antihistamine market. The FDA updated labeling in 2023 to require warnings about 12 high-risk drug classes. Kaiser Permanente’s automated drug alerts cut antihistamine-related ER visits by 34% between 2020 and 2022.Research is moving toward drugs with zero off-target effects. Levocetirizine (Xyzal) and bilastine are already better. In the future, pharmacogenomic testing may identify people who metabolize diphenhydramine slowly - and warn them before they take it.
For now, the message is simple: if you’re taking more than one sedating drug, ditch the Benadryl. Your brain - and maybe your life - depends on it.


Comments (13)
Benadryl is a trap. I used to take it for sleep until I woke up confused and falling off my bed. Switched to Zyrtec and never looked back. Game changer.
I didn't realize how many of my meds were anticholinergic until I ran the UW calculator. Between my blood pressure pill, bladder med, and nightly Benadryl, I was at ACB 5. My doctor was shocked. We cut two of them out and I feel like I got my brain back. Why isn't this common knowledge?
People still take Benadryl like it's candy? Bro. You're not a 1970s college kid. Your liver doesn't work like it did back then. Stop being lazy and get a real allergy med. This isn't rocket science.
Just want to say I took diphenhydramine with my SSRI for weeks and had zero issues. Maybe I'm just lucky? I know it's risky but not everyone reacts the same. Also, I think the FDA warnings are kinda overblown - most people aren't mixing 5 different sedatives.
It’s almost poetic how we’ve turned medicine into a Russian roulette game where the only prize is dementia. We’re not just medicating ourselves - we’re curating our own cognitive decline with a side of OTC convenience. The real tragedy? We’re proud of it. "I take Benadryl and it works!" Yes. And so does cyanide. But you wouldn’t snack on that, would you?
Big Pharma doesn’t want you to know this because second-gen antihistamines cost more. They push Benadryl because it’s cheap and addictive. My grandma died after mixing it with her heart meds. The hospital said "unfortunate interaction" - but I know it was corporate greed. They even make kids’ Benadryl in fruit flavors. That’s not medicine - that’s a trap for grandparents. And don’t get me started on how they hide the warnings in tiny font. They want you dead quietly.
It is imperative that individuals consult with their primary care physician prior to combining any pharmacological agents, particularly those with central nervous system depressant properties. This is a matter of clinical safety.
The author's reliance on anecdotal Reddit data and Amazon ratings as primary evidence is methodologically unsound. While the clinical implications are valid, the presentation lacks scholarly rigor. One might argue that this is a disservice to the public's understanding of pharmacology.
I used to think Benadryl was my best friend - until I nearly crashed my car after one drink and a pill. Now I take Allegra, sleep like a baby, and my brain doesn't feel like mush. It's not magic - it's just smarter choices. You got this. Swap it out today. Your future self will high-five you.
Wow. Another fear-mongering article that makes me want to stop taking medicine entirely. Next you'll tell me aspirin causes bleeding and water gives you water intoxication. People die from falling down stairs too - should we ban stairs? This isn't science, it's panic dressed up as advice.
Thank you for this! 🙏 I'm from India and many here still use diphenhydramine as a sleep aid - even doctors prescribe it. I shared this with my uncle who was on 7 meds including Benadryl. He switched to loratadine and now he's alert, walking without help, and even gardening again. Small change, huge difference. 🌿
So true! 🇮🇳 In my village, everyone uses Benadryl for colds, allergies, and sleep. No one knows about ACB scores. This post should be translated into Hindi and Tamil. We need to wake up before it's too late. 🙏
Actually, the CDC data is misleading. Most of those respiratory depression cases involved polypharmacy with alcohol and opioids - not just antihistamines. Blaming Benadryl is like blaming forks for obesity. The real issue is people being dumb, not the drug. Also, I've taken it with Xanax for years. Fine.