Fluoroquinolone-NSAID Risk Calculator
Risk Assessment
This tool calculates your increased risk of acute kidney injury when taking fluoroquinolone antibiotics with NSAIDs based on your kidney function and age.
Your risk assessment will appear here...
What This Means
When fluoroquinolone antibiotics and NSAIDs are combined, the risk of acute kidney injury increases significantly. The FDA reports that the risk is 3.5 times higher compared to using fluoroquinolones alone (which already carries a 2x risk).
Critical Warning
Combining these drugs can cause permanent kidney damage that may require dialysis. If you're currently taking both medications, contact your doctor immediately if you experience any of these symptoms:
- Reduced urine output
- Swelling in ankles or face
- Extreme fatigue
- Confusion or difficulty concentrating
Safer Alternative
For pain or fever relief while taking fluoroquinolone antibiotics, use acetaminophen (Tylenol). It doesn't affect kidney blood flow and is the only safe pain reliever to use with these antibiotics.
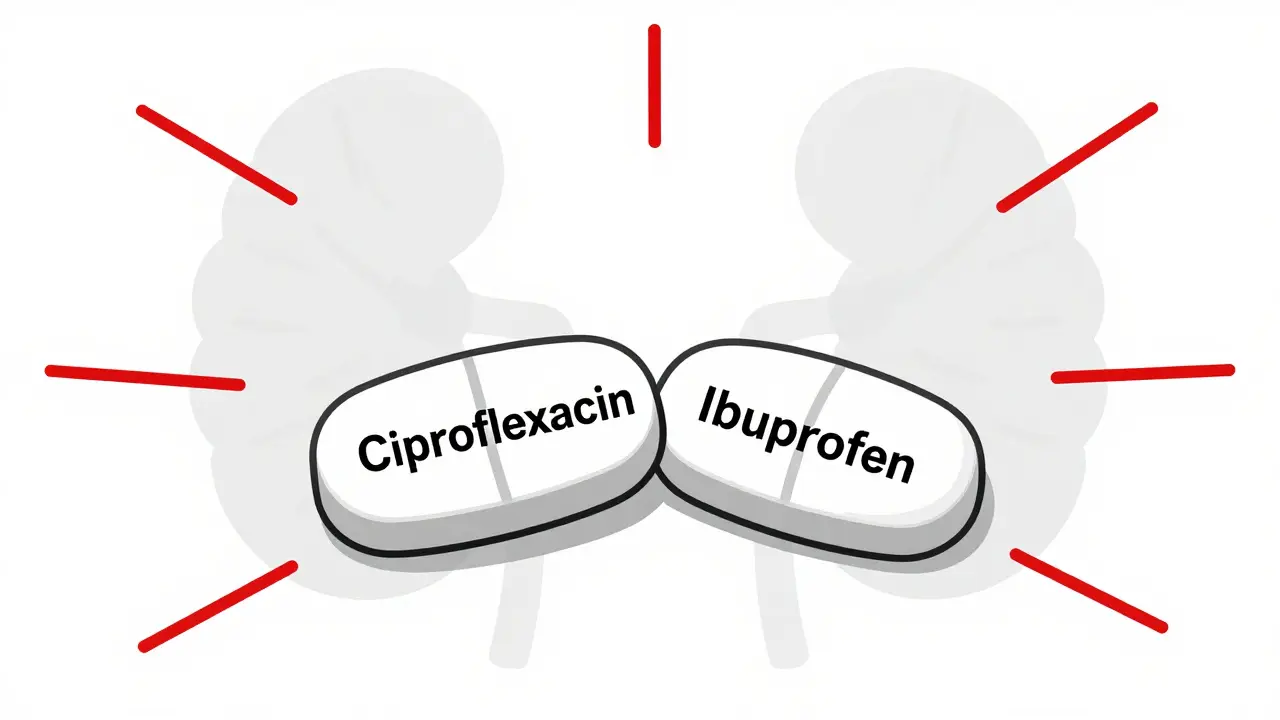
When you're prescribed an antibiotic like ciprofloxacin or levofloxacin for a stubborn infection, and your doctor also recommends ibuprofen or naproxen for pain or fever, it’s easy to assume these drugs are safe together. But the truth is, combining fluoroquinolone antibiotics with NSAIDs can significantly raise your risk of serious, sometimes permanent, damage to your brain and kidneys. This isn’t theoretical. It’s documented in medical journals, flagged by health regulators worldwide, and confirmed by real patient stories.
What Are Fluoroquinolone Antibiotics?
Fluoroquinolones are a class of powerful antibiotics that include ciprofloxacin, levofloxacin, moxifloxacin, norfloxacin, and ofloxacin. They’ve been used since the 1980s to treat everything from urinary tract infections to pneumonia. But they’re not gentle drugs. Unlike penicillin or amoxicillin, which target bacteria more selectively, fluoroquinolones interfere with bacterial DNA replication in a way that can also disrupt human cells-especially in the nervous system and kidneys.
The U.S. FDA, Health Canada, and the European Medicines Agency have all issued multiple warnings since 2016. These agencies now say fluoroquinolones should be reserved for infections with no other treatment options. Why? Because even a short course-sometimes just five to seven days-can trigger side effects that last months or years. These include tendon ruptures, nerve pain, muscle weakness, and cognitive issues like brain fog or memory loss.
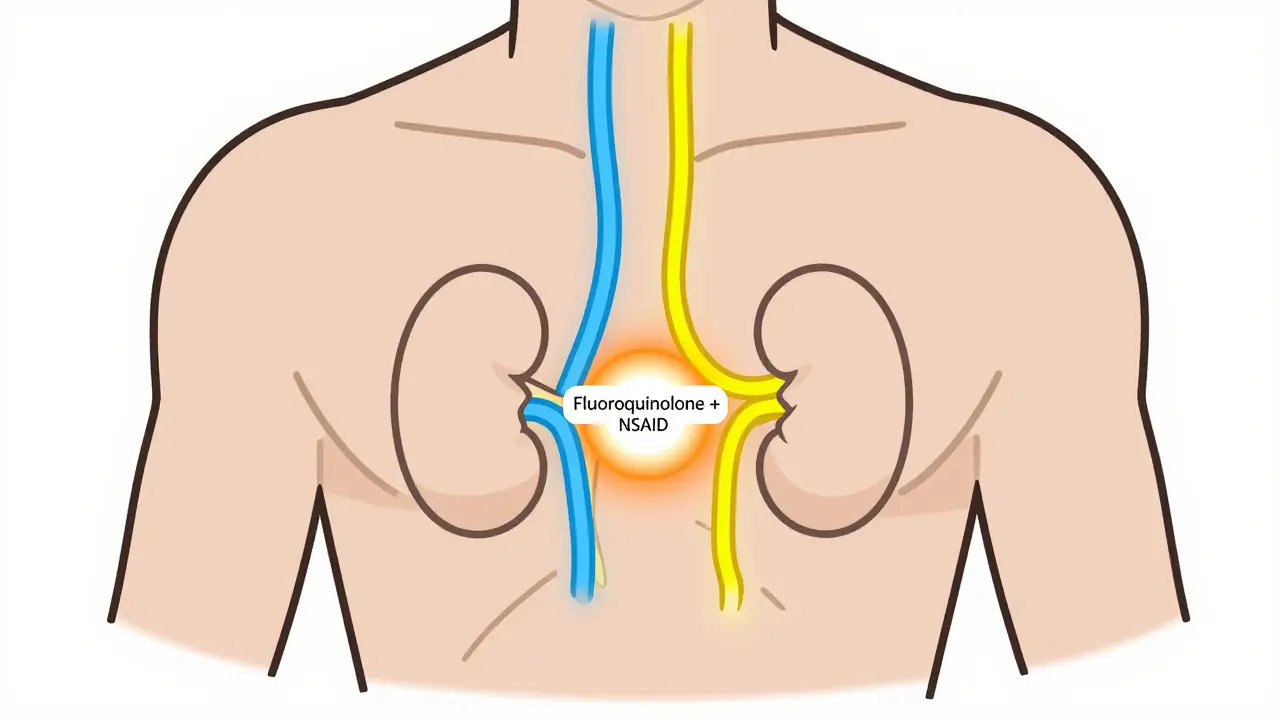
The Kidney Risk: When Two Drugs Become One Threat
Your kidneys filter your blood. They’re responsible for removing waste and keeping your electrolytes balanced. Both fluoroquinolones and NSAIDs stress this system-but together, they’re far worse.
Fluoroquinolones can cause acute interstitial nephritis, a condition where immune cells invade kidney tissue, leading to swelling and reduced function. They can also trigger crystalluria, where drug crystals form in the urine and block tiny tubes in the kidneys. NSAIDs, on the other hand, reduce blood flow to the kidneys by blocking prostaglandins, chemicals that help maintain kidney function, especially when you’re dehydrated or older.
Studies show that taking fluoroquinolones alone increases your risk of hospitalization for acute kidney injury by about two times. Add an NSAID, and that risk jumps to 3.5 times higher-especially in people over 60 or those with existing kidney problems. A 2013 study in JAMA Internal Medicine found that elderly patients on both drugs were far more likely to need dialysis or suffer lasting kidney damage.
One case from the UK’s Yellow Card system involved a 58-year-old man who took ciprofloxacin and ibuprofen for a UTI. His creatinine level-normally around 82-spiked to 287 in just a few days. His kidneys never fully recovered. He still has chronic kidney disease 18 months later.
Neurological Damage: More Than Just a Headache
Most people know NSAIDs can cause dizziness or headaches. But few realize they can also trigger rare cases of aseptic meningitis-brain inflammation without infection. Fluoroquinolones are even more concerning. They cross the blood-brain barrier and interfere with GABA receptors, the brain’s main calming system. At the same time, they activate NMDA receptors, which excite nerve cells. This imbalance can lead to seizures, confusion, hallucinations, or even psychosis.
Levofloxacin is especially linked to seizures and delirium. Ciprofloxacin often causes confusion and memory lapses. Even people with no history of mental health issues have reported sudden personality changes after taking these drugs. In patients with reduced kidney function, these drugs build up in the bloodstream. If your eGFR is below 60, fluoroquinolone levels can rise by 50-100%. That means even standard doses become toxic.
Combine that with NSAIDs, which also affect brain chemistry, and you’re stacking two neurotoxic agents on top of each other. The result? Higher chances of prolonged brain dysfunction. Patients report lasting trouble concentrating, emotional numbness, or insomnia that doesn’t go away after stopping the drugs.
Real People, Real Consequences
Behind the statistics are real lives changed. The Fluoroquinolone Effects Research Foundation surveyed over 1,200 patients. Seventy-eight percent said their symptoms lasted more than six months. Thirty-two percent said they were permanently disabled. One woman from Melbourne described how, after a course of levofloxacin and naproxen for a sinus infection, she developed severe nerve pain in her hands and feet, brain fog so bad she couldn’t read a book, and chronic fatigue. Three years later, she still can’t work full-time.
Online communities like Reddit’s r/FQAntibioticDamage have over 14,500 members. Their stories are chillingly similar: sudden tendon pain, tingling in the limbs, anxiety attacks, and cognitive decline-all starting within days of taking a fluoroquinolone, often with an NSAID.
What Should You Do Instead?
If you need an antibiotic and also need pain relief, you don’t have to choose between infection control and safety.
- For pain or fever: Use acetaminophen (paracetamol). It doesn’t affect kidney blood flow or interact with fluoroquinolones. It’s the safest option.
- For UTIs: Ask about nitrofurantoin or fosfomycin. They’re just as effective for simple infections and carry far fewer risks.
- For respiratory infections: Amoxicillin-clavulanate or doxycycline are often better first choices than fluoroquinolones.
- For chronic conditions: If you’re on long-term NSAIDs for arthritis or back pain, avoid fluoroquinolones entirely. Your doctor should have a backup plan.
Also, make sure your doctor checks your kidney function before prescribing fluoroquinolones. A simple blood test for creatinine and eGFR takes minutes. If your eGFR is below 60, they should avoid these drugs unless absolutely necessary.

Regulatory Changes Are Happening-But Slowly
Since 2017, regulators have tightened restrictions. Health Canada now requires warning labels about disabling side effects. The UK’s MHRA says fluoroquinolones should only be used when no other options exist. The FDA has updated labels to include warnings about mitochondrial damage, a possible root cause of long-term neurological and kidney injury.
Prescriptions have dropped by 22% in the U.S. since 2015. But fluoroquinolones are still overused-especially in countries like India and China, where they’re sold without prescription. In Australia, they remain widely available, but GPs are increasingly cautious.
The economic cost is huge: fluoroquinolone-related side effects cost the U.S. healthcare system $1.8 billion a year. Kidney injuries make up 37% of that. Neurological damage adds another 29%. That’s billions spent treating preventable harm.
When to Say No
You have the right to ask questions. If your doctor prescribes a fluoroquinolone, ask:
- Is this the only option?
- Have you checked my kidney function?
- Can I use acetaminophen instead of ibuprofen?
- What are the signs of nerve or kidney damage I should watch for?
If you’re already on both drugs, don’t stop abruptly. Talk to your doctor. But do not assume it’s safe just because it’s common. The risks are real, and they’re growing.
Fluoroquinolones aren’t evil drugs. They save lives when used correctly. But they’re not for every infection. And they’re never safe with NSAIDs unless you’re under strict medical supervision-and even then, the risks may outweigh the benefits.
Can fluoroquinolones and NSAIDs cause permanent damage?
Yes. Both fluoroquinolones and NSAIDs can cause lasting harm, especially when taken together. Fluoroquinolones are linked to peripheral neuropathy, tendon rupture, and kidney damage that may not fully reverse. NSAIDs can cause chronic kidney disease with long-term use. When combined, the risk of permanent kidney injury and neurological symptoms like chronic pain, brain fog, or muscle weakness increases significantly. Many patients report symptoms lasting over a year, and some never fully recover.
Are all fluoroquinolones equally dangerous?
No. While all fluoroquinolones carry risks, some are more likely to cause neurological side effects than others. Levofloxacin and ciprofloxacin are most commonly linked to seizures, confusion, and delirium. Moxifloxacin has a higher risk of heart rhythm issues. Ofloxacin appears to have slightly lower neurotoxic potential, but it still carries the same kidney risks. No fluoroquinolone is truly safe when paired with an NSAID.
What are safer alternatives to fluoroquinolones for a UTI?
For uncomplicated urinary tract infections, nitrofurantoin and fosfomycin are preferred first-line options. They’re just as effective, have fewer side effects, and don’t interact dangerously with NSAIDs. For more serious infections, amoxicillin-clavulanate or cephalosporins like cefdinir are often better choices. Always ask your doctor if a safer alternative exists before accepting a fluoroquinolone.
Can I take acetaminophen with fluoroquinolones?
Yes. Acetaminophen (paracetamol) is the safest pain reliever to use with fluoroquinolones. It doesn’t affect kidney blood flow or interfere with the antibiotic’s metabolism. Unlike NSAIDs, it doesn’t raise the risk of acute kidney injury or neurological side effects. If you need fever or pain relief while on ciprofloxacin or levofloxacin, acetaminophen is the recommended choice.
How do I know if I’m having a bad reaction?
Watch for sudden changes: tingling or burning in your hands or feet, unexplained muscle weakness, swelling in your ankles, reduced urine output, confusion, hallucinations, or seizures. If you develop any of these symptoms within days of starting either drug, stop taking them and contact your doctor immediately. Don’t wait. Early recognition can prevent permanent damage.

Comments (9)
OMG I literally just had this happen to me 😭 I took cipro + ibuprofen for a UTI last year and woke up with tingling in my fingers like I’d been electrocuted… then my brain just… stopped working for months. I couldn’t read a sentence without forgetting what it said. I’m still recovering. Why isn’t this on every prescription label?? 🫠
Let me cut through the fluff - this isn’t ‘risk,’ it’s a goddamn medical crime. Fluoroquinolones are basically chemical scalpels with no off-switch, and pairing them with NSAIDs is like lighting a match in a gas station. The FDA’s warnings are toothless because Big Pharma still pushes these like candy. I’m a pharmacist. I’ve seen 17-year-olds on levofloxacin for sinus infections. That’s not medicine - that’s corporate negligence dressed in a white coat. And yes, the kidney damage? Permanent. The brain fog? Often lifelong. Stop normalizing this.
While the concerns raised in this post are valid and well-documented, I would encourage readers to consider the broader context. Fluoroquinolones remain life-saving in cases of multidrug-resistant infections, sepsis, or complicated pyelonephritis. The key is not blanket avoidance, but appropriate patient selection, renal function assessment, and avoidance of concurrent NSAIDs in vulnerable populations. The data supporting the interaction is robust - but so is the clinical utility when used judiciously. Shared decision-making, not fear, should guide therapy.
Oh wow. Another ‘doctor is evil’ post. Let me guess - you took antibiotics for a cold and now you think your soul is broken? People, we’ve had antibiotics since the 1940s. If this were as catastrophic as you claim, hospitals would be full of walking zombies. You’re not ‘damaged,’ you’re anxious. And no, acetaminophen isn’t magic - it just doesn’t make you feel like you’re dying so you blame the drugs. Chill.
Thank you for this comprehensive breakdown. The combination of fluoroquinolones and NSAIDs is one of the most under-discussed dangers in outpatient care. What’s especially troubling is how often this happens in urgent care settings - where a provider prescribes cipro for a ‘possible UTI’ without a culture, then throws in ibuprofen because ‘it’s just a painkiller.’ The reality? Many patients aren’t even told about the interaction. I’ve counseled dozens who didn’t know NSAIDs could amplify neurotoxicity. This needs to be part of standard patient education - not an afterthought. Acetaminophen is the obvious, safe alternative. Simple. Effective. Underused.
YOOOO I JUST GOT MY CIPRO RX AND I WAS ABOUT TO GRAB IBUPROFEN FROM MY CABINET 😱 THANK YOU FOR THIS POST!! I’M SWITCHING TO TYLENOL RIGHT NOW!! MY KIDNEYS ARE SWEARING THEY’RE THANKFUL 😭😭😭 ALSO - WHY IS THIS NOT ON EVERY SINGLE MEDICATION BOTTLE?? LIKE?? WHY IS THIS STILL A SECRET??
Western medicine’s obsession with chemical sledgehammers. In India, we’ve used turmeric, neem, and garlic for infections for 5000 years. You guys take a pill for a sneeze and then wonder why your kidneys give up. Fluoroquinolones? More like fluoro-quit-your-life. NSAIDs? Just add water and wait for the dialysis. You don’t need a PhD to see this is a scam. The real question: who profits? Hint: not you.
Yeah yeah, ‘permanent damage.’ I’ve been on cipro 3x and I’m fine. You’re just one of those people who Google symptoms and think you have a rare disease. My grandma took cipro + naproxen for 2 weeks and she’s still hiking. You’re not special. Stop fearmongering.
Acetaminophen? Really? That’s your solution? You’re not a doctor. You’re a blog post. Real doctors know when to use the big guns. If you’re scared of antibiotics, go live in a cave. And stop pretending NSAIDs are evil. They’re just misunderstood. Also - your ‘14,500 Reddit members’ aren’t a study. They’re a cult.