When your gallbladder stops working right, the pain doesn’t just come and go-it hits like a wave you can’t swim through. Imagine a sudden, sharp grip under your right ribs that lasts for hours, maybe with fever, yellowing skin, or nausea that won’t quit. This isn’t just indigestion. It’s your bile system screaming for help. Gallbladder and biliary diseases affect 10-15% of adults in developed countries, and for many, it starts with stones.
What Are Gallstones, Really?
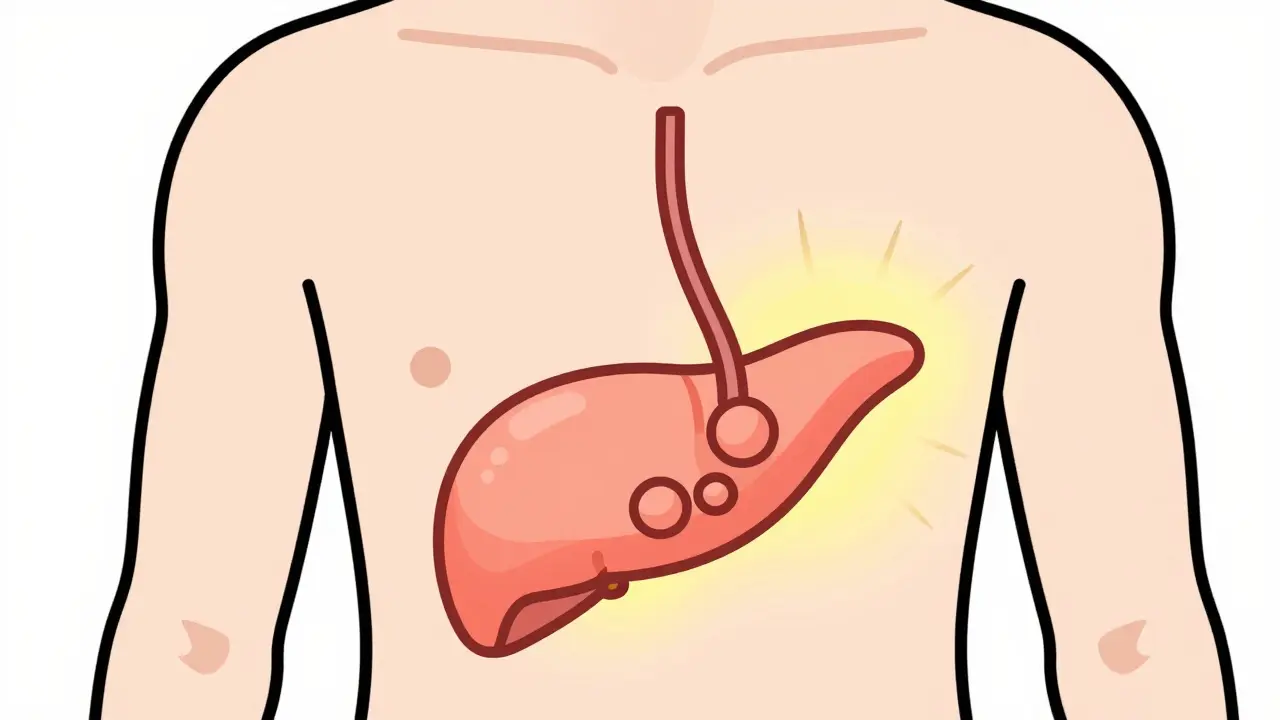
Gallstones aren’t just lumps of junk. They’re crystals formed inside your gallbladder when bile gets out of balance. About 80% are made of cholesterol, the same kind found in your blood. The other 20% are pigment stones, mostly bilirubin, a breakdown product of red blood cells. Mixed stones fall in between. These stones can be as small as grains of salt or as big as golf balls.Most people with gallstones never know they have them. In fact, the American College of Gastroenterology says asymptomatic stones don’t need treatment. The risk of complications from surgery is higher than the chance those stones will cause trouble-only about 1-2% of people with silent stones develop symptoms each year. But when they do, it’s serious. Blockage of the cystic duct leads to acute cholecystitis-inflammation of the gallbladder. Blockage in the common bile duct? That’s when things get dangerous.
Cholangitis: When Infection Hits the Bile Duct
Cholangitis is a bacterial infection of the bile ducts. It’s not common, but it’s life-threatening. The classic signs? Charcot’s triad: severe pain in the upper right abdomen, fever, and jaundice (yellow skin or eyes). If you add confusion or low blood pressure, you’re looking at Reynolds’ pentad-a sign of septic shock.Most cases happen because a gallstone gets stuck in the common bile duct, trapping bacteria that normally live in the gut. These bugs multiply fast in the blocked, stagnant bile. Without treatment, mortality can hit 10-20%. That’s why doctors don’t wait. If you have these symptoms, you need urgent care.
It’s also why ERCP isn’t just a test-it’s often an emergency procedure. In the U.S., over 500,000 hospital admissions each year are tied to complications from gallstones, including cholangitis and pancreatitis. And women are affected more than men-2.1 times more often. Why? Hormones. Estrogen increases cholesterol in bile, and pregnancy, birth control, and hormone therapy all raise the risk.
ERCP: The Procedure That Fixes Blocked Ducts
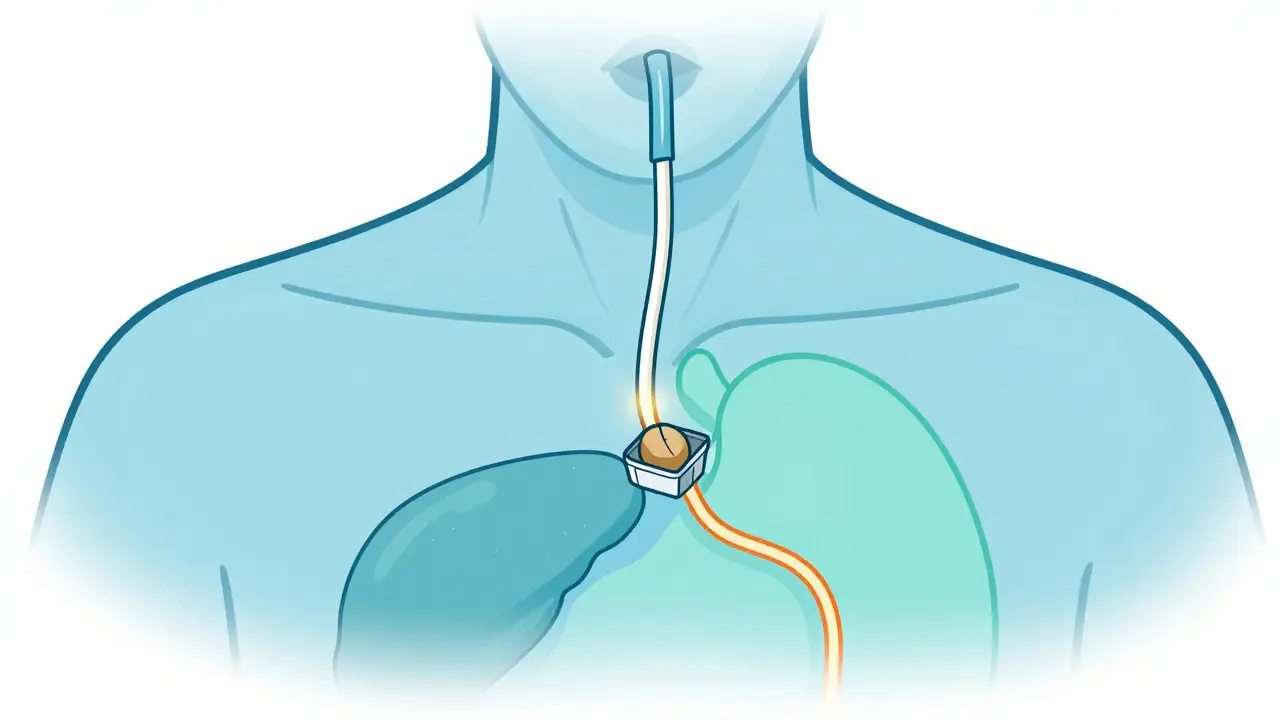
Endoscopic Retrograde Cholangiopancreatography, or ERCP, is a hybrid procedure-part endoscopy, part X-ray, part surgery. A thin, flexible tube with a camera is passed through your mouth, down your throat, into your stomach, and into the first part of your small intestine. There, the doctor finds the opening where the bile duct empties-the ampulla of Vater.They inject dye, take X-rays, and look for stones or narrowing. If they find a stone blocking the duct, they use tiny tools to cut the muscle around the opening (sphincterotomy), grab the stone with a basket, or break it up. Success rates? 85-95% in experienced hands. It’s the gold standard for removing bile duct stones.
But it’s not risk-free. About 3-10% of patients develop post-ERCP pancreatitis-the most common complication. It happens when the procedure irritates the pancreas. Some patients need to stay in the hospital for days. That’s why experts now recommend using MRCP (magnetic resonance cholangiopancreatography) first. MRCP is non-invasive, has 95% sensitivity, and doesn’t carry the same risks. Only if MRCP shows stones should you go ahead with ERCP.
And here’s a critical gap: only 30-40% of patients with bile duct stones get ERCP done at the same time as their gallbladder removal. That means many people go through two surgeries, two recoveries, and two sets of risks. Better coordination between surgeons and gastroenterologists could cut that number in half.
What About Other Treatments?
You might hear about pills to dissolve stones. Ursodeoxycholic acid (UDCA) can work-but only for small cholesterol stones under 15mm. Even then, it takes 6-12 months and only works in 30-40% of cases. And it does nothing for pigment stones. Plus, stones come back in 50% of people within five years if the gallbladder stays in place.Shock wave therapy? Used to be popular. Now it’s rarely used. It breaks stones into pieces, but those pieces often get stuck and cause more blockages. Recurrence rates are too high.
Laparoscopic cholecystectomy-removing the gallbladder through small cuts-is the go-to for symptomatic gallstones. It’s done in 90% of cases. Recovery? Most people go home in 1-2 days and back to work in 7-10 days. Compare that to open surgery: 4-6 weeks off work, a long scar, and more pain.
After gallbladder removal, some people get diarrhea. Not everyone. About 10-15% report ongoing loose stools, especially after fatty meals. That’s because bile flows continuously into the intestine instead of being stored. Most adjust within weeks. Some need loperamide or a low-fat diet for months. It’s not dangerous, but it’s inconvenient.
Who’s at Risk?
Gallstones aren’t random. Certain groups are far more likely to get them:- Women: Especially after pregnancy, on birth control, or hormone therapy.
- Over 60: Risk jumps to 25% in older adults.
- Obese: BMI over 30 doubles or triples your risk.
- Rapid weight losers: Losing more than 1.5kg per week ups your chance.
- Diabetics: Two to three times more likely to develop stones.
- Native Americans: Up to 64% of Pima Indians have gallstones-the highest rate in the world.
- Asian populations: Higher rates of pigment stones due to diet and genetics.
Even cirrhosis increases your risk by 4-6 times. That’s because liver damage changes how bile is made and processed.
What Happens After ERCP or Surgery?
Recovery isn’t just about healing-it’s about adjusting. After ERCP, you’ll have a sore throat from the scope. That lasts a few days. You’ll be monitored for pancreatitis signs: abdominal pain, nausea, fever. Most people go home the same day if all’s well.After gallbladder removal, you’ll be told to eat low-fat for 2-4 weeks. Then, slowly reintroduce fats. Most people resume normal eating by 6 weeks. But here’s the truth: you don’t need to avoid fat forever. Your liver still makes bile. It just doesn’t store it. So you might need to eat smaller meals and avoid large amounts of fried food.
Some patients develop post-cholecystectomy syndrome-persistent pain or bloating after surgery. That happens in about 12% of cases. It could be from leftover stones, bile duct injury, or even functional gut issues. If it lasts, you need more tests.
What’s New in 2026?
Technology keeps improving. In 2023, the FDA approved a new duodenoscope with a fully disposable elevator. That’s huge. Between 2013 and 2018, faulty scopes caused 112 outbreaks of drug-resistant infections. Now, the part that bends and moves is single-use-no more cleaning nightmares.Intraductal ultrasound (IDUS) is also gaining ground. It uses a tiny ultrasound probe inside the bile duct during ERCP. It spots stones under 5mm that standard imaging misses. Sensitivity jumps to 92% from 75%.
Researchers are now working on drugs to dissolve pigment stones-something that doesn’t exist yet. Right now, if you have pigment stones, surgery or ERCP is your only option.
Telehealth follow-ups after ERCP are cutting readmissions by 18% in pilot programs. Patients get a video check-in on day 2 or 3. If they have pain or fever, they’re seen right away. No waiting until it’s bad.
What Should You Do If You Suspect a Problem?
If you have sudden, severe pain under your right ribs, especially with fever or yellow skin:- Go to the ER. Don’t wait.
- Ask for an ultrasound first. It’s quick, safe, and finds gallstones in 84% of cases.
- If the bile duct is suspected, ask about MRCP-not ERCP yet.
- If stones are found in the duct, make sure your surgeon and endoscopist coordinate. Same-day ERCP during cholecystectomy saves you from a second procedure.
- Don’t push for surgery if you have no symptoms. Watchful waiting is safer.
And if you’ve had your gallbladder out and still have issues? Don’t assume it’s normal. Talk to your doctor. There are answers.
It’s not just about removing a stone or a gallbladder. It’s about understanding how your body moves bile, why it gets blocked, and how to prevent complications before they become emergencies. Knowledge is the best tool you have.

Comments (11)
The government is hiding the real cause of gallstones-it’s not cholesterol or diet, it’s fluoride in the water. They’ve known since the 80s but kept it quiet because gallbladder surgery brings in billions. I’ve seen it in my own family. Three women, all on birth control, all had stones after the town changed the water supply. No one talks about it because Big Pharma owns the AMA. You think ERCP is healing you? It’s just a money pump. They’ll keep you coming back for ‘follow-ups’ while the real toxin stays in your system.
Okay but like… 🤔 have you ever thought that maybe the gallbladder isn’t just a ‘storage unit’ but a *sacred organ* that holds emotional toxicity? I mean, right under the ribs-right where we hold our anger, right? 🌊✨ I had mine out and I swear, my mood improved 300%. No more ‘I hate my job’ fits. It’s not just bile-it’s *unprocessed trauma*. The body is a temple, and your gallbladder? It’s the priest who’s been holding all your rage. Let it go. 🙏💛
Hey everyone, I just want to say how amazing it is that we’re finally talking about this in such a clear way! 💪 I had my gallbladder out last year after years of ignoring the pain-I thought it was just ‘bad digestion’-and now I’m living my best life! Yes, I still get loose stools sometimes after pizza, but guess what? I’m alive, I’m active, and I’m not scared to eat again. You’re not broken-you’re just adjusting. Take it slow, hydrate, and be kind to yourself. You’ve got this! 🌈💖 And if you’re scared about surgery? I was too. But my surgeon was a rockstar. Ask questions. Be your own advocate. You’re stronger than you think!
So let me get this straight-we’re spending half a million hospital visits a year on something that’s basically a plumbing issue… and the solution is cutting out a perfectly good organ? 🤨 Also, ‘watchful waiting’ is the new ‘just drink more water’? Yeah, I’ll just sit here and hope my gallstone doesn’t turn into a tiny, angry dictator. Also, ERCP is risky but MRCP is ‘safer’? So we’re just going to scan it to death before doing the thing that fixes it? Classic. I’m just glad I’m not the one getting poked with a scope.
Actually, the 80% cholesterol stone stat is misleading. Most of those are from people who eat low-fat diets and take statins-your body overproduces cholesterol when you deprive it of fat. The real culprit? Processed ‘healthy’ foods. Also, ‘asymptomatic stones don’t need treatment’? Tell that to the woman who died of sepsis from a ‘silent’ stone. And why is everyone ignoring that MRCP misses 5% of stones? I’ve seen cases where the stone was right there, but the radiologist said ‘no findings.’ So now we’re replacing one risk with another? And don’t even get me started on the ‘low-fat diet after surgery’ myth. That’s what they told my aunt. She got worse. Fat is fuel. Bile is a detergent. You need both. Stop listening to doctors who think butter is the devil.
This is very important. Everyone should know about gallstones. If you feel pain, go to doctor. Do not wait. Your body is trying to tell you something. Eat healthy, drink water, move your body. You can be strong. You can be healthy. You are not alone. I believe in you. 💕
From a hepatobiliary perspective, the pathophysiological cascade initiated by biliary stasis and bacterial translocation in cholangitis is fundamentally rooted in endotoxin-mediated TLR4 activation, leading to NF-kB-driven cytokine storm. The current standard of care-ERCP with sphincterotomy-remains the most efficacious intervention, but the 3–10% post-ERCP pancreatitis rate remains suboptimal. The emerging utility of IDUS for sub-5mm stone detection represents a paradigm shift, though its cost-effectiveness in resource-limited settings remains unvalidated. Also, the 64% prevalence in Pima populations is not merely genetic-it’s epigenetic, tied to thrifty genotype expression under modern caloric abundance.
Wait, so if MRCP has 95% sensitivity, why do we still do ERCP first in some cases? I’ve read conflicting guidelines. And is the ‘same-day ERCP during cholecystectomy’ really that common? My surgeon said it’s ‘not always feasible’-but I’m wondering if that’s just a scheduling issue. Also, I’ve heard some docs skip MRCP entirely because insurance won’t cover it. Is that a thing? Just… curious. 😅
I just want to say-this post was so clear, so thoughtful, and honestly, it made me feel less alone. I had cholangitis last year. I thought I was dying. I was scared to even breathe. And the doctors? They didn’t explain anything. They just said ‘you need ERCP’ and handed me a consent form. I didn’t know what bile ducts were. I didn’t know what ‘sphincterotomy’ meant. I just knew I was in pain. Reading this? It helped me understand what happened to me. Thank you. I’m still adjusting, still getting diarrhea sometimes, but I’m alive. And I’m grateful. If you’re reading this and you’re scared? You’re not alone. We’re all here. You’ve got this. ❤️
Okay, but if estrogen increases cholesterol in bile, then why is it that men who take testosterone replacement therapy also get gallstones at higher rates? And why do men who’ve had prostate cancer and are on anti-androgens get them even more? And why do transgender women on HRT have a 4x higher incidence than cis men? And why is no one talking about this? Also, the ‘2.1 times more often in women’ stat ignores that women are more likely to get diagnosed because they’re more likely to go to the doctor. Men just suffer silently until they collapse. And then we call it ‘sudden death.’ It’s not a gender issue-it’s a diagnostic bias issue. Also, what about the 15% of people who get stones without any of these risk factors? Are they just… cursed?
Just got my gallbladder out last month. Still sore. Still eating tiny meals. But I’m alive. And I’m not mad anymore. Just… tired. Thanks for writing this. I didn’t know half of this. I thought it was just ‘bad luck.’ Turns out, it was my diet, my stress, and my mom’s genes. I’m gonna tell my sister to get checked. She’s got all the risk factors. Thanks for the info. 😊