Lithium Toxicity: Signs, Risks, and What to Do If You Suspect It
When you take lithium, a mood-stabilizing drug used primarily for bipolar disorder. Also known as lithium carbonate, it helps control extreme mood swings—but the line between therapeutic and toxic levels is thin. Many people take it safely for years, but even small mistakes—like skipping a dose, getting dehydrated, or starting a new medication—can push lithium into dangerous territory.
Lithium toxicity, a buildup of lithium in the bloodstream to harmful levels doesn’t happen overnight. It often creeps in slowly. Early signs include hand tremors, frequent urination, nausea, or feeling unusually tired. If you ignore these, symptoms can worsen: confusion, muscle weakness, slurred speech, or even seizures. It’s not rare—studies show up to 1 in 5 people on long-term lithium experience at least one mild toxic episode. What makes it risky is that the symptoms look a lot like the condition it’s meant to treat, so people often dismiss them as "just my bipolar acting up." But this isn’t your mood cycling—it’s your body warning you.
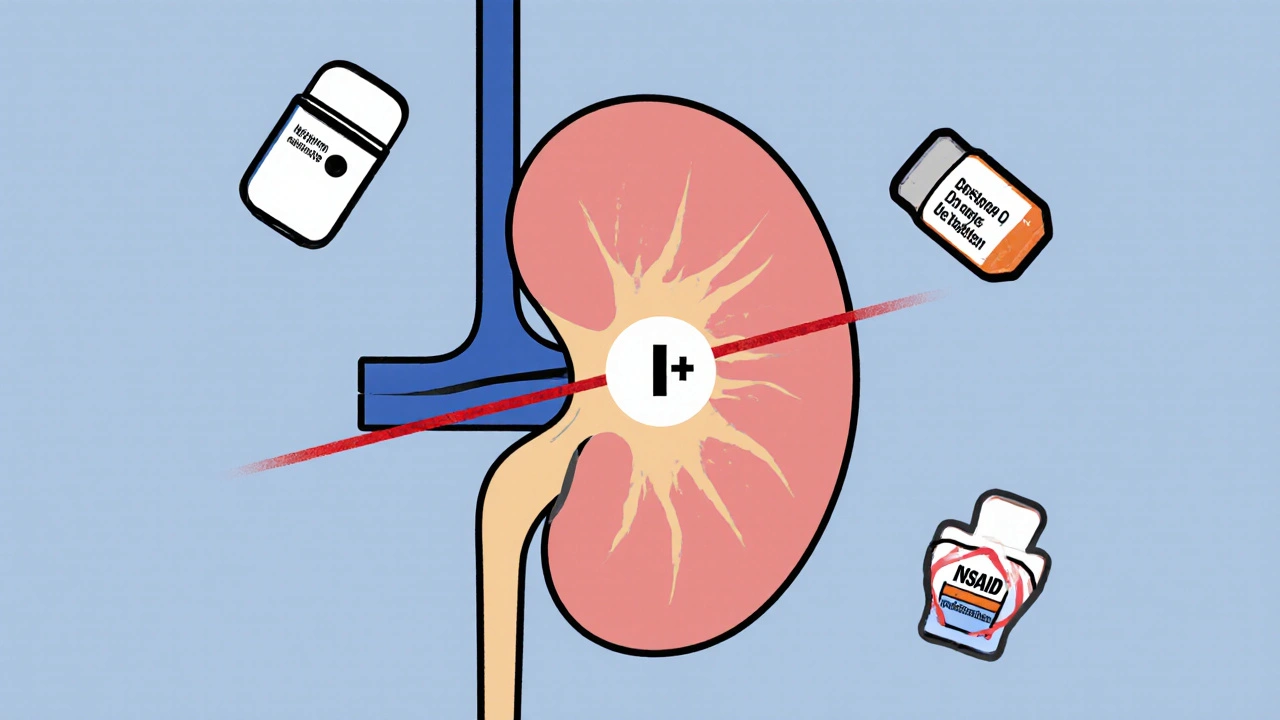
Lithium levels, the amount of lithium in your blood measured through routine blood tests are the only reliable way to know if you’re in danger. Doctors usually check them every few months, but if you’re sick, sweating a lot, or on new meds like NSAIDs or diuretics, you need a test sooner. Many people don’t realize that dehydration, even mild, can spike lithium levels by 20% or more. A hot day, a bad stomach bug, or cutting back on water can turn a safe dose into a medical emergency.
You’re not alone if you’ve worried about this. Thousands of people manage lithium successfully, but it takes attention. You need to know your body’s signals, stick to your dosing schedule, and speak up when something feels off. The posts below cover real cases, common drug interactions that raise lithium risk, how to monitor yourself at home, and what to do if you think you’re experiencing toxicity. No fluff. No guesswork. Just what you need to stay safe while taking this powerful medication.
- November 20, 2025
- Comments 17
- Medications and Supplements