Lithium Toxicity Risk Calculator
Current Lithium Level
Medications
Results
Estimated Lithium Level: mmol/L
Current Risk Level:
Recommended Actions
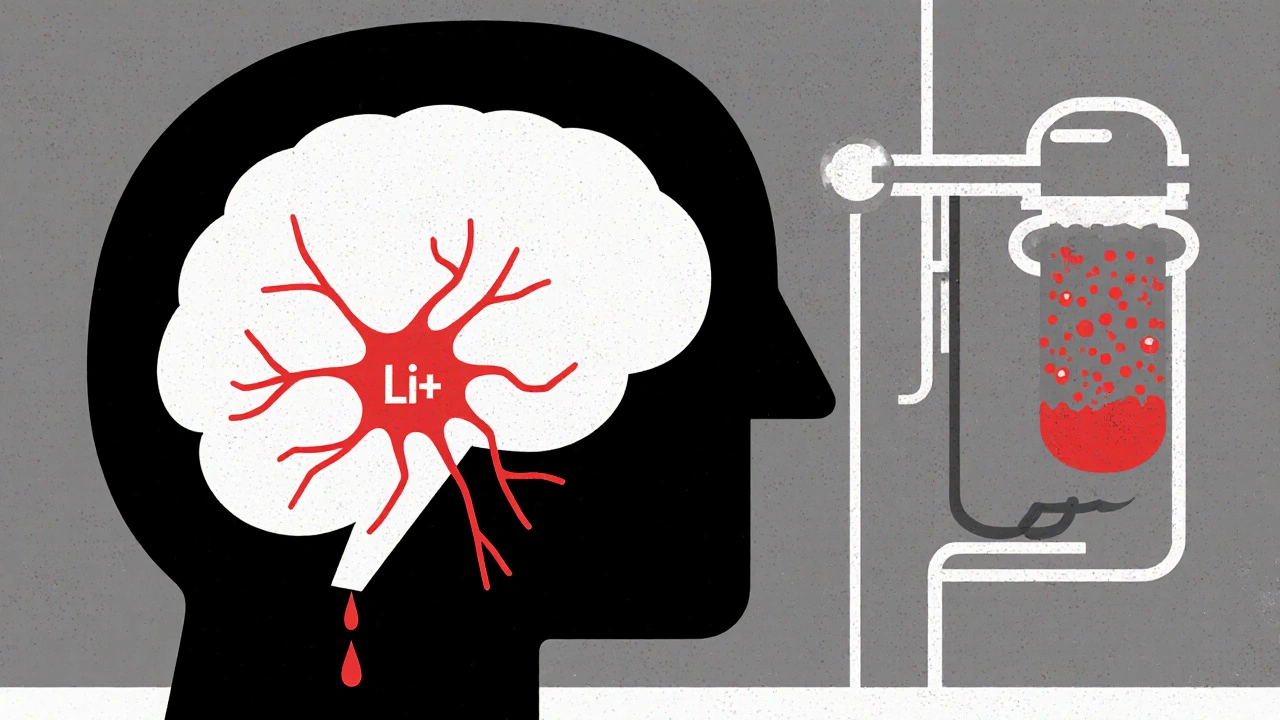
For people taking lithium to manage bipolar disorder, even a small change in their body’s chemistry can turn a safe medication into a dangerous one. Lithium has a razor-thin line between helping and harming - a therapeutic range of just 0.6 to 1.2 mmol/L. Go above 1.5 mmol/L, and symptoms like tremors, confusion, and nausea start showing up. Above 2.5 mmol/L, and you’re in a medical emergency. The problem isn’t the lithium itself. It’s what else you’re taking - especially common drugs like diuretics and NSAIDs.
Why Lithium Is So Sensitive
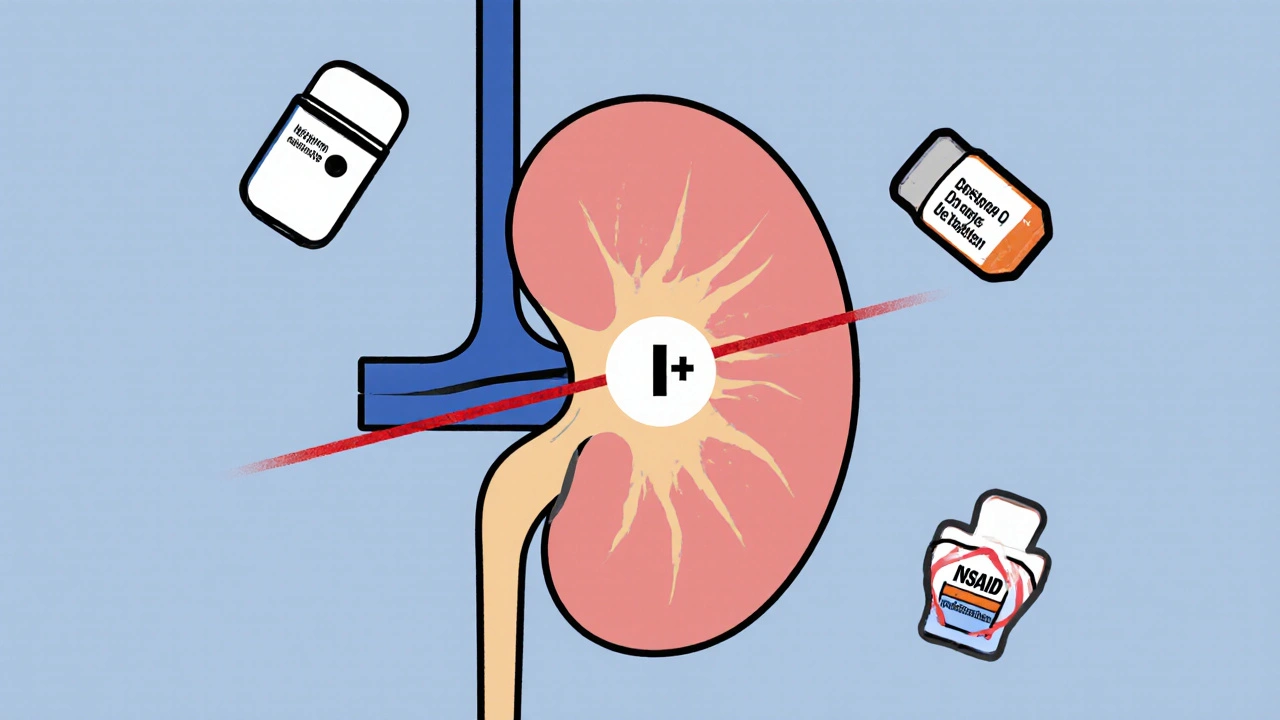
Lithium doesn’t get broken down by your liver. It doesn’t bind to proteins. It doesn’t linger in tissues. Instead, it rides through your bloodstream and gets filtered out by your kidneys - almost entirely. That’s why anything that changes how your kidneys work can throw off lithium levels. Your kidneys reabsorb lithium along with sodium. When sodium levels drop, your kidneys hang on tighter to lithium. That’s where diuretics and NSAIDs come in.Diuretics: The Silent Lithium Triggers
Diuretics - often called water pills - are prescribed for high blood pressure, heart failure, or swelling. But not all diuretics affect lithium the same way.Thiazide diuretics like hydrochlorothiazide and bendroflumethiazide are the worst offenders. They act on a part of the kidney where lithium gets reabsorbed. Even a low dose - 25 mg of hydrochlorothiazide daily - can raise lithium levels by 25% to 40%. In some cases, levels have spiked fourfold. This isn’t rare. Studies show 75% to 85% of patients on thiazides and lithium see dangerous increases. The rise often happens within 3 to 5 days. Many people don’t notice symptoms until it’s too late.
Loop diuretics like furosemide are less risky, but still dangerous. They increase lithium levels by 10% to 25%, especially in people with reduced kidney function (eGFR under 60). Furosemide is sometimes used on purpose in patients with lithium-induced nephrogenic diabetes insipidus - a condition where the kidneys can’t concentrate urine. But even then, levels must be checked every few days.
There’s no safe diuretic when you’re on lithium. But if you absolutely need one, furosemide is the lesser evil. Still, your doctor should lower your lithium dose by 20% to 25% and check your blood levels every 4 to 5 days for the first month.
NSAIDs: The Over-the-Counter Danger
NSAIDs - ibuprofen, naproxen, diclofenac - are taken by millions for headaches, arthritis, or back pain. What most people don’t realize is that these common painkillers can turn a stable lithium dose into a toxic one.NSAIDs block prostaglandins in the kidneys. Prostaglandins help keep blood flow steady to the filtering units. When they’re blocked, the kidneys filter less blood. That means less lithium gets cleared. The result? Lithium builds up.
The risk varies by drug:
- Indomethacin: Increases lithium by 20% to 40% - the strongest interaction.
- Piroxicam: 20% to 30% increase.
- Naproxen: 15% to 25% increase.
- Ibuprofen: 15% to 20% increase - and it’s sold over the counter.
- Celecoxib: Only 5% to 10% increase - the safest NSAID option if you must use one.
Here’s the scary part: people take ibuprofen and naproxen without telling their doctor. They think it’s just an occasional pill for a headache. But even a few days of use can push lithium into toxic territory. A 2017 case in New Zealand documented a 72-year-old woman who died after starting an NSAID. Her lithium level jumped from 0.8 to 1.9 mmol/L in just seven days. She had no warning signs until it was too late.
Other Drugs That Can Raise Lithium Levels
It’s not just diuretics and NSAIDs. Other common medications can interfere too:- ACE inhibitors (like lisinopril) - raise levels by 15% to 25%.
- ARBs (like valsartan) - increase levels by 10% to 20%.
- Calcium channel blockers (like verapamil) - don’t raise lithium levels much, but can worsen side effects like tremors and ringing in the ears.
- Some antidepressants - especially SSRIs like fluoxetine - can also increase lithium levels, though less predictably.
And don’t forget herbal supplements. There’s not enough data to say any are safe with lithium. Ginger, ginkgo, or St. John’s wort could interact in ways we don’t yet understand.
What Happens When Lithium Goes Toxic
Toxicity isn’t always obvious. Early signs include:- Hand tremors that get worse
- Frequent urination or thirst
- Nausea, vomiting, or diarrhea
- Slurred speech or confusion
- Muscle weakness or twitching
As levels climb above 2.0 mmol/L, symptoms become neurological: seizures, loss of coordination, or even coma. Levels above 2.5 mmol/L are life-threatening. Standard treatment includes stopping lithium, giving fluids, and monitoring closely. But here’s the catch: even when blood levels drop, lithium stays trapped inside brain and nerve cells. That’s why severe cases often need hemodialysis - not just to clear the blood, but to pull lithium out of tissues. One case report showed a patient needed multiple dialysis sessions because lithium kept leaking back into the bloodstream from cells.
How to Stay Safe
If you’re on lithium, here’s what you need to do:- Never start a new medication without checking with your doctor - even an OTC painkiller.
- Get your lithium level checked before starting any new drug, and again 4 to 5 days after.
- If you’re prescribed a diuretic or NSAID, your lithium dose should be lowered by 15% to 25% upfront.
- Monitor your symptoms. If you feel off, get tested - don’t wait.
- Use celecoxib instead of ibuprofen if you need an NSAID.
- Ask for furosemide instead of hydrochlorothiazide if you need a diuretic.
- Keep a list of all your meds - including supplements - and share it with every doctor you see.
Many patients don’t realize their doctor isn’t automatically checking their lithium levels every time they refill a prescription. You have to be your own advocate. Ask: “Have you checked my lithium level since I started this new pill?”
New Tools Are Coming
There’s hope on the horizon. In 2023, the FDA approved a home-monitoring device called LithoLink™ - a small device you use like a glucose meter. It tests your lithium level with a finger prick and sends results directly to your doctor. Early users report better adherence and fewer hospital visits.Researchers are also testing a new form of lithium - nano-encapsulated citrate - that’s less dependent on kidney function. In trials, it showed 40% less fluctuation when taken with ibuprofen. This could change everything for people who need both lithium and pain relief.
Final Reality Check
Lithium is one of the most effective mood stabilizers we have. It cuts suicide risk by nearly half compared to placebo. But that power comes with responsibility. The interaction risks aren’t theoretical - they’re deadly. Every year, people end up in emergency rooms because they took Advil for a headache and didn’t realize it could poison them.The solution isn’t to avoid lithium. It’s to treat it with the respect it demands. Know your numbers. Know your meds. Ask questions. And never assume a drug is “too common” to be dangerous.
Can I take ibuprofen if I’m on lithium?
It’s not recommended. Ibuprofen can raise lithium levels by 15% to 20%, which can push you into toxicity. If you need pain relief, talk to your doctor first. They might suggest celecoxib, which has a much weaker interaction, or a non-drug option like heat therapy or physical therapy. Never take ibuprofen regularly without monitoring your lithium levels every 4 to 5 days.
What’s the safest diuretic to take with lithium?
Furosemide (Lasix) is safer than thiazide diuretics like hydrochlorothiazide. Thiazides cause lithium levels to spike in up to 85% of patients. Furosemide raises levels by only 10% to 25%, and only in people with kidney issues. Still, your doctor should reduce your lithium dose by 20% to 25% and check your levels every 4 to 5 days after starting furosemide. Never self-prescribe diuretics if you’re on lithium.
How often should lithium levels be checked when starting a new drug?
When you start a drug that interacts with lithium - like an NSAID or diuretic - levels should be checked within 4 to 5 days. After that, weekly checks for the first month are standard. Once stable, monitoring can go back to every 3 to 6 months. But if your dose changes, you get sick, or you start another new medication, restart the 4- to 5-day check cycle. Don’t wait for symptoms - toxicity can happen fast.
Can herbal supplements interact with lithium?
There’s not enough research to say any herbal supplement is safe with lithium. Some, like St. John’s wort, may affect kidney function or alter drug metabolism. Others, like ginger or ginkgo, could increase bleeding risk or interfere with blood pressure control - which indirectly affects lithium clearance. Always tell your doctor about every supplement you take, even if you think it’s harmless.
What should I do if I think I’m experiencing lithium toxicity?
Stop taking lithium immediately and seek medical help. Don’t wait for a doctor’s appointment - go to the emergency room. Symptoms like confusion, severe tremors, vomiting, or slurred speech mean you need urgent care. Blood tests will confirm your lithium level, but treatment shouldn’t wait for results. You may need IV fluids, and in severe cases, hemodialysis to remove lithium from your tissues. Even if you feel better after a day, follow up - lithium can rebound from cells into your bloodstream hours later.

Comments (17)
Okay, but let’s be real-why is the FDA letting Big Pharma get away with this? Lithium’s been around since the 1940s, and we’re only now getting a home monitor? That’s not innovation, that’s negligence. And don’t even get me started on celecoxib being the ‘safe’ NSAID-pharma’s favorite magic bullet. Meanwhile, people are dying because their doctor assumed ‘it’s just Advil.’
My cousin took ibuprofen for a migraine and ended up in ICU. No one warned her. No one checked her levels. And now? She’s on dialysis three times a week. This isn’t medical advice-it’s a death sentence wrapped in a prescription pad.
They call it ‘therapeutic range’ like it’s a spa day. It’s not. It’s walking a tightrope over a pit of acid. And we’re supposed to trust doctors who don’t even know what’s in their own formulary?
They need mandatory alerts in every EHR. Every time someone prescribes an NSAID to a lithium patient, the system should scream. Like, sirens. Red lights. A goddamn alarm clock that won’t shut up until the pharmacist calls the patient.
I’m not mad. I’m just… done.
you guys!! i just found out my dr gave me hydrochlorothiazide last month and i’ve been on lithium for 5 years!! 😱 i’m so scared but i called them right away and they lowered my dose!! thank you for this post!! i feel like i almost died but now i know what to watch for!! 🙏💛
I almost died. Twice.
Let me guess-this whole thing was funded by the LithoLink™ investors. You’re selling fear to push a $300 gadget that probably doesn’t work any better than a $5 urine strip. And don’t even get me started on ‘nano-encapsulated citrate.’ Sounds like a sci-fi drug from a 2002 anime. You think they’re not just trying to patent lithium again so they can jack up the price? Lithium carbonate costs $10 a month. The new version? $800. You think I’m wrong?
And why is everyone acting like NSAIDs are the enemy? I’ve been taking ibuprofen for 12 years with lithium and I’m fine. My levels are stable. Maybe it’s not the drugs-it’s the people who don’t get their blood tested. Blame the system, not the pills.
Also, ‘St. John’s wort could interfere’? Really? That’s the best you’ve got? You’re scaring people into avoiding natural remedies while letting Big Pharma off the hook. Classic.
This is one of the most important posts I’ve read all year. Thank you for laying this out so clearly. So many people are on lithium and have no idea how fragile their balance is. I’ve worked in mental health for 18 years, and I’ve seen too many avoidable ER visits because someone took ‘just one’ Advil.
One thing I’d add: if you’re on lithium, keep a small notebook. Write down every medication, supplement, or even herbal tea you take. Bring it to every appointment-even the dermatologist. Most doctors don’t ask about OTC stuff unless you bring it up.
And if you’re feeling off-tremors, nausea, fuzzy head-don’t wait. Call your psychiatrist immediately. Don’t say ‘I’ll wait till Monday.’ You don’t get a Monday if your lithium hits 2.0.
You’re not being paranoid. You’re being smart.
They don’t want you to know this, but lithium is a controlled substance in disguise. The government lets it fly under the radar because it’s cheap. But if it were a new patent drug? It’d be $1,200 a month. They’re letting people die so they can keep the profits on the fancy new ‘nano’ version. And don’t even get me started on the fact that the FDA approved LithoLink™ after one small trial with 47 patients. That’s not science-that’s corporate theater.
I’ve been on lithium for 11 years. I’ve had three near-fatal spikes. All from NSAIDs. All preventable. All ignored.
They don’t care. They’re just waiting for you to become a statistic so they can sell you the next ‘breakthrough.’
How do we know the 75-85% stat for thiazides is accurate? What study? Was it randomized? Double-blind? Controlled for renal function? I’ve read the FDA’s 2019 review on lithium interactions-it doesn’t cite those numbers. And the ‘fourfold increase’ case-was that in a patient with CKD? Dehydrated? On a low-sodium diet? The post reads like a fear-mongering pamphlet, not a clinical guide.
Also, why is celecoxib ‘safer’? Because it’s a COX-2 inhibitor? But COX-2 inhibitors have higher CV risk. So we’re trading heart attacks for kidney toxicity? That’s not a win. That’s a trade-off. And nobody’s talking about it.
This isn’t education. It’s emotional manipulation.
bro i was on lithium for like 3 years and i used to take ibuprofen like it was candy. one time i got really dizzy after a headache and went to urgent care-they checked my levels and i was at 1.8. they were like ‘dude, you almost died.’
now i only use heat packs or tylenol (acetaminophen) and i check my levels every 3 months. also i keep a list of meds on my phone. it’s not hard, just be aware. you’re not alone.
They’re hiding something. Lithium isn’t dangerous-it’s being weaponized. Why do you think the VA and Medicare push it so hard? Because it’s cheap. And because if you’re on lithium, you’re easier to control. You can’t just ‘quit’ it. You need a 3-week taper. You need blood tests. You need to be monitored.
Think about it: the same people who tell you to ‘take your meds’ are the ones who won’t let you switch to something natural. They want you dependent. They want you scared of Advil. They want you scared of water pills. They want you scared of your own body.
This isn’t medicine. It’s control.
lithium is just a metal right? why we are even taking it? why not meditation? or yoga? or ayurveda? in india we have been using brahmi and ashwagandha for centuries for mood stability. why we are relying on toxic chemicals? is this capitalism? or brainwashing? i think we lost our connection with nature
also who says 0.6-1.2 is the only range? maybe our bodies are different? maybe science is wrong? maybe lithium is not the answer but the problem
As someone who’s been on lithium for 8 years, I can say this: knowledge saves lives. I take furosemide for edema and my doctor lowered my lithium dose by 25% before I even started it. We checked levels every 5 days for a month. No drama. No crisis.
And yes, celecoxib is the way to go if you need NSAID. I’ve used it for years. No issues. But the key is communication. Tell your doctor EVERYTHING-even if you think it’s ‘just ginger tea.’
This isn’t about fear. It’s about responsibility. And we all have a role to play.
Let me clarify something: lithium toxicity is 100% preventable with proper monitoring. The problem isn’t the drugs-it’s the lack of coordination between prescribers. Your psychiatrist knows about lithium. Your rheumatologist doesn’t. Your dentist doesn’t. Your mom gives you ibuprofen for a headache and says ‘it’s fine.’
That’s the real issue: fragmented care. The solution isn’t new gadgets-it’s better communication protocols. Electronic health records need mandatory lithium interaction flags. Pharmacies need mandatory alerts. Patients need a lithium wallet card-like a diabetic ID.
And yes, St. John’s wort is dangerous. I’ve seen a patient go from 0.9 to 1.9 in 48 hours after starting it. No one told the psychiatrist. No one told the pharmacist. That’s on us.
Stop blaming Big Pharma. Start demanding better systems.
Thank you for writing this with such clarity. I’ve been on lithium for 15 years, and I’ve had two near-misses-both from NSAIDs. I didn’t know the risk until I read a study in the Journal of Clinical Psychiatry. That’s when I started keeping a medication log and asking every new provider: ‘Is this safe with lithium?’
I’ve also switched to celecoxib and furosemide. It’s not about fear. It’s about empowerment. You don’t have to be a medical expert to protect yourself. Just be consistent. Be curious. Be vocal.
And if you’re reading this and you’re on lithium? You’re not alone. We’re in this together.
Hey, I just wanted to say-did you know that lithium is used in batteries? Like, the same lithium? So… is your brain just a battery? And are they slowly draining it with NSAIDs? I mean… think about it. We’re literally using the same element to power our phones and our moods. That’s wild. And kinda terrifying.
Also, I think the government is replacing lithium with something else in the water supply. I saw a documentary. They said it’s to ‘calm the population.’ I don’t know. Just saying.
Interesting perspective. In Nigeria, many do not have access to regular blood tests, yet lithium remains widely prescribed. The real issue is not just drug interactions but systemic neglect. Without access to monitoring, even the safest regimen becomes dangerous. We need global awareness-not just technical guidelines. The human cost is invisible in wealthy nations because it is hidden behind clinics and labs. In ours, it is buried in silence.
My brother died from this. No one told him.
That’s heartbreaking. Thank you for sharing. His story should be heard.