Generic Drug Savings Calculator
How Much Can You Save?
Calculate the difference between brand-name and generic drug costs. Remember: Generics provide identical therapeutic benefits at a fraction of the cost.
Enter values to see your potential savings.
Ever wondered why the pill you receive looks nothing like the one on the TV ad, yet the pharmacist says it works the same? That’s the generic‑vs‑brand debate, and the answer lives in the label and the science behind therapeutic equivalence.
When you pick up a prescription, the label might read Generic drugs, but the tablet could be a different color, shape, or size. The brand‑name counterpart - think Brand-name drugs like Lipitor - carries a trademarked look and a proprietary name. Both contain the same active pharmaceutical ingredient (API) in the same strength, but they differ in marketing, appearance, and price.
What the FDA Requires for Both Forms
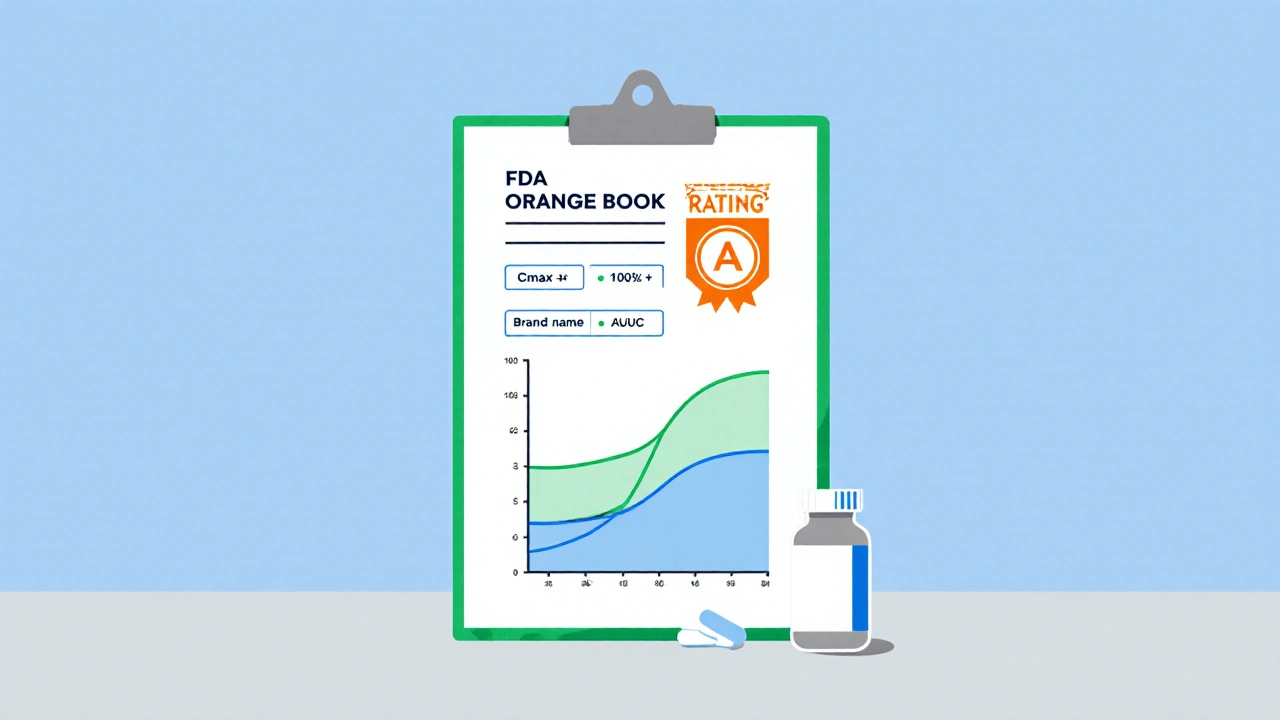
The U.S. Food and Drug Administration (FDA) sets a single safety net for all prescription medicines. Under the Hatch‑Waxman Act of 1984, manufacturers file an Abbreviated New Drug Application (ANDA) to prove a product matches the reference listed drug. The FDA’s Orange Book lists each approved drug, its dosage form, and an “A” rating that signals therapeutic equivalence.
Key requirements are identical:
- Same API quantity and strength
- Same route of administration (tablet, injection, etc.)
- Equivalent pharmacological effect
- Matching labeling for indications, dosage, warnings, and adverse reactions
What can change? Inactive ingredients - the excipients like fillers, binders, and dyes - may differ because trademark law forces generics to look distinct. The FDA does not require identical colors or shapes, just that the therapeutic performance stays the same.
Labeling Rules: Names and Appearance
Brand‑name labels flaunt a proprietary name (Prilosec for omeprazole) and a distinctive logo. Generic labels must display the chemical name of the API (omeprazole) and any approved synonyms. The FDA’s 2021 Guidance for Industry mandates that every section of the label - from indications to contraindications - mirrors the brand’s wording word‑for‑word.
Appearance is the other visible difference. Trademark law obliges generics to avoid the same color, shape, or imprint, which is why a generic aspirin might be round and pink while the brand is oval and white. This visual shift can cause confusion, but it does not affect how the drug works.
Therapeutic Equivalence and Bioequivalence
The cornerstone of the generic claim is bioequivalence. The FDA requires that the generic’s pharmacokinetic parameters - Cmax (peak concentration) and AUC (area under the curve) - fall within 80‑125 % of the brand’s values in a study of 24‑36 healthy volunteers. That 20 % window is tighter than the natural batch‑to‑batch variation you see even within a single brand.
When the study passes, the FDA awards an “A” rating in the Orange Book, meaning doctors and pharmacists can safely substitute the generic for the brand. Studies, such as the 2021 JAMA Internal Medicine analysis of two million cardiovascular patients, found no difference in outcomes between generic and brand prescriptions.
Cost Savings and Market Impact
Price is the headline grabber. Generic versions typically cost 80‑85 % less than their brand counterparts. For example, atorvastatin (Lipitor) averaged $375.22 per month in brand form in Q2 2023, while the same dose at Walmart was $4.00. The Association for Accessible Medicines reports that generics represent 90 % of prescriptions but only 25 % of total drug spend, saving the U.S. health system $1.67 trillion from 2007‑2016 and $313 billion annually today.
Even with these savings, generics make up just 24 % of total prescription expenditures because brand‑name drugs dominate high‑cost categories like oncology and biologics. The market is still growing: the 2022 IQVIA report valued the U.S. generic market at $127.4 billion, up 3.2 % from the prior year.
When Generics May Not Be a Straight‑Swap
Not every drug is a perfect fit for automatic substitution. Narrow therapeutic index (NTI) drugs - such as warfarin, levothyroxine, and phenytoin - have a tiny margin between effective and toxic levels. The FDA advises close monitoring when switching between generics of NTI drugs, especially if the patient’s lab values are unstable.
Complex molecules also pose challenges. Biologics and insulin analogues often require a specific delivery device, making true generics (biosimilars) harder to produce. As of 2023, only a handful of insulin biosimilars have FDA approval, and many providers still prefer the original brand due to familiarity and device consistency.

How Pharmacists Handle Substitution
In 49 states, pharmacists can automatically replace a brand prescription with a generic unless the prescriber writes “Dispense as Written.” The substitution process involves three quick checks:
- Confirm the Orange Book “A” rating for the drug.
- Verify that the patient isn’t on an NTI drug that needs special monitoring.
- Document the switch in the pharmacy’s system and inform the patient about appearance changes.
Most clinicians feel comfortable with generics; a 2022 AMA survey showed 94 % of physicians routinely prescribe them. When a switch involves multiple generic manufacturers, pharmacists may advise a short trial period and watch for any new side‑effects.
Label and Equivalence Comparison
| Aspect | Brand‑Name Drug | Generic Drug |
|---|---|---|
| Proprietary name | Trademarked (e.g., Lipitor) | Chemical name (e.g., atorvastatin) |
| Appearance | Trademarked color/shape | Different color/shape, no trademark |
| Inactive ingredients | Specific fillers, dyes | Can vary between manufacturers |
| Therapeutic equivalence rating | Not applicable (reference) | Orange Book “A” rating when approved |
| Cost (average US retail) | ~$375/month (Lipitor example) | ~$4/month (generic atorvastatin) |
Frequently Asked Questions
Do generic drugs work the same as brand‑name drugs?
Yes. The FDA requires generic drugs to be bioequivalent, meaning they deliver the same amount of active ingredient into the bloodstream as the brand product.
Why do generics look different?
Trademark law forces generic manufacturers to avoid the exact color, shape, or imprint of the brand. The difference is cosmetic only.
Are there drugs that shouldn’t be substituted?
Narrow therapeutic index drugs like warfarin, levothyroxine, and some anti‑epileptics need close monitoring when switched. Your doctor may request “Dispense as Written.”
How much can I save by choosing a generic?
On average, generics cost about 10‑20 % of the brand price. In high‑volume drugs like statins, the difference can be over 99 %.
What should I do if I notice a new pill shape?
Check the label for the same active ingredient and strength. If it matches, it’s a generic equivalent. Call your pharmacist if you’re unsure.
Bottom line: generic drugs give you the same therapeutic punch as the name‑brand version, just at a fraction of the cost. Knowing the label rules, bioequivalence standards, and the few exceptions helps you and your provider make confident, money‑saving choices.


Comments (8)
Generic drugs are just as safe and effective as their brand counterparts when approved.
The FDA’s bioequivalence criteria hinge on Cmax and AUC metrics that must sit within an 80‑125 % confidence interval.
The statistical window is actually tighter than the batch‑to‑batch variability you see in brand‑name production.
In practice, the pharmacokinetic profile of a generic pill mirrors that of its reference listed drug.
Manufacturers achieve this by conducting crossover studies with healthy volunteers under fasting conditions.
The data are then submitted in an Abbreviated New Drug Application, or ANDA, which the agency reviews for completeness.
Once approved, the product earns an “A” rating in the Orange Book, signaling therapeutic equivalence.
The label, down to the indication wording, must be word‑for‑word identical to the brand reference.
Inactive excipients like binders or dyes can differ, but they are not supposed to affect the drug’s pharmacodynamics.
For most patients, switching between a brand and its generic will feel indistinguishable.
The cost differential is the real driver, with generics often costing less than 15 % of the brand price.
Insurance formularies frequently mandate generic substitution unless a prescriber writes “dispense as written.”
Some clinicians still prefer brand products for narrow therapeutic index drugs such as levothyroxine.
Nonetheless, large‑scale outcome studies, including a 2021 JAMA analysis, have not shown any clinically meaningful difference in efficacy or safety.
The evidence base backs the regulatory stance that generics are a safe, cost‑effective alternative.
Bottom line: if your pharmacist offers a generic, you’re getting the same therapeutic punch at a fraction of the cost 😊
Great summary, Nic! I really appreciate how you broke down the bioequivalence process step by step.
Your explanation of the “A” rating and the label requirements makes it clear why clinicians trust generics.
It’s also reassuring to see the data from large studies reinforcing safety.
For anyone worried about switching, this paints a confident picture.
Thanks for sharing such a thorough and accessible overview.
Ah yes, the mysterious pill‑shifting conspiracy – how dare the FDA let us save money on colorless tablets!
Clearly the pharmaceutical giants are trying to keep us in the dark about the true power of those “inactive ingredients.”
One might wonder if the tiny differences in excipients are a covert signal from the Illuminati of medicine.
But of course, the “orange book” is just a cover for their secret agenda, right?
In any case, enjoy your cheap meds while the elite watch from their ivory towers.
Seeing the numbers on cost savings really puts things in perspective – generics can be 80‑90 % cheaper than brand‑name drugs.
When insurers push for generics, patients often see a dramatic drop in out‑of‑pocket expenses.
That’s why it’s worth checking your pharmacy’s label for the same active ingredient.
Even with a different shape or color, the therapeutic effect remains unchanged.
Just a heads‑up: keep an eye on any new side‑effects when you switch manufacturers.
Thanks for the practical tips, Kasey.
I’ve seen many patients feel nervous when their pills look different, even though they’re equivalent.
It helps to reassure them that the FDA’s bioequivalence standards are rigorous.
And reminding them to talk to their pharmacist if anything feels off is always a good idea.
Hope everyone feels more confident about making the switch.
All this hype about generics being “just as good” is nonsense – you can’t trust a pill that looks nothing like the original.
The differences in fillers and dyes can affect absorption, especially for sensitive patients.
I’ve heard stories of people experiencing side‑effects after switching to a cheap copy.
Pharma companies do a decent job, but the regulatory shortcuts make me skeptical.
Brands invest in research and quality; generics are just a money‑saving gimmick.
While concerns about excipients are understandable, extensive pharmacokinetic studies demonstrate that variations in inactive ingredients do not materially alter bioavailability for most oral solid dosage forms.
The FDA’s requirement that Cmax and AUC remain within 80‑125 % of the reference product is designed precisely to address such issues.
Moreover, post‑marketing surveillance data have not identified a systematic safety signal attributable to generic substitution.
Therefore, the assertion that generics are inherently inferior lacks empirical support.