Medication Appetite Impact Calculator
How Your Medication Affects Appetite
Select your medication to see potential appetite changes and receive personalized management recommendations.
Many people start a new medication expecting relief from their symptoms-better sleep, lower blood pressure, improved mood-but they don’t expect to feel hungrier than ever, or suddenly lose interest in food altogether. Appetite changes from medication are more common than most realize, and they can happen fast. One person might gain 10 pounds in two months on a new antidepressant. Another might struggle to eat enough on a psychiatric drug that makes food taste bland. These aren’t just inconveniences-they can derail health goals, worsen chronic conditions, and lead to real medical risks.
Why Your Medication Is Changing Your Appetite
It’s not random. Your appetite is controlled by a complex system in your brain, mainly the hypothalamus, which responds to signals from hormones like ghrelin (hunger) and leptin (fullness). Many medications interfere with this system by altering brain chemicals-serotonin, dopamine, histamine, and others-that directly influence hunger and cravings. For example, second-generation antipsychotics like olanzapine and quetiapine boost ghrelin levels by 15-20% within weeks. That means your body thinks it’s starving, even when it’s not. Antidepressants like mirtazapine work similarly, increasing appetite by affecting histamine receptors. On the flip side, stimulants like amphetamines suppress appetite by flooding your system with norepinephrine and dopamine, making food feel unappealing. Even common drugs like beta-blockers or antihistamines can nudge your hunger signals in subtle but meaningful ways. The effect isn’t always the same. Some people lose weight on antidepressants at first, then gain it back after a year. That’s because short-term use often increases serotonin, which reduces impulsivity and makes you feel full. But over time, your brain adapts. Serotonin receptors downregulate, and suddenly, you crave carbs-especially sugary or starchy foods-to get that quick mood lift. It’s not weakness. It’s biology.Which Medications Are Most Likely to Cause Appetite Changes?
Not all drugs affect appetite the same way. Some are notorious for weight gain. Others might help you lose it. Here’s what the data shows:- High risk of weight gain: Olanzapine (Zyprexa), risperidone (Risperdal), quetiapine (Seroquel), mirtazapine (Remeron), amitriptyline, insulin, sulfonylureas (like glipizide), lithium, and diphenhydramine (Benadryl).
- Moderate risk: Paroxetine (Paxil), fluoxetine (Prozac) after long-term use, propranolol, and thiazolidinediones (pioglitazone).
- Weight-neutral or weight-loss: Bupropion (Wellbutrin), topiramate (Topamax), metformin, vortioxetine (Trintellix), and liraglutide (Saxenda).
For example, mirtazapine causes weight gain in 40% of users within six months-many gain more than 7% of their body weight. Meanwhile, bupropion leads to weight loss in about 25% of users, with no change in the rest. Topiramate, originally an anti-seizure drug, is now used off-label for weight control because it reduces cravings and makes people feel full faster. In studies, 60% of users lost 3-5 kg in six months.
Even diabetes meds tell a story: insulin often adds 2-4 kg in the first six months. Metformin? It usually leads to a 2-3 kg loss. That’s why guidelines now recommend metformin as first-line for people with prediabetes who are overweight.
What Real People Are Experiencing
Online communities are full of stories that mirror the clinical data. On Reddit, threads about quetiapine and weight gain have thousands of upvotes. One user shared gaining 30 pounds in four months-just from a sleep aid prescribed after a panic attack. Another described how olanzapine made them feel “hungry all the time, even after eating a full plate.” But there are success stories too. A woman on MyMoodMonitor switched from mirtazapine to bupropion and lost 15 pounds over six months without her depression getting worse. Another man started drinking a glass of water before every meal and found his portion sizes dropped by 13%. He didn’t even need to change his food. These aren’t outliers. A survey of 1,450 people taking olanzapine found that 72% reported constant hunger-the most frustrating side effect by far. And 65% said it was harder to manage than anxiety or sleep problems.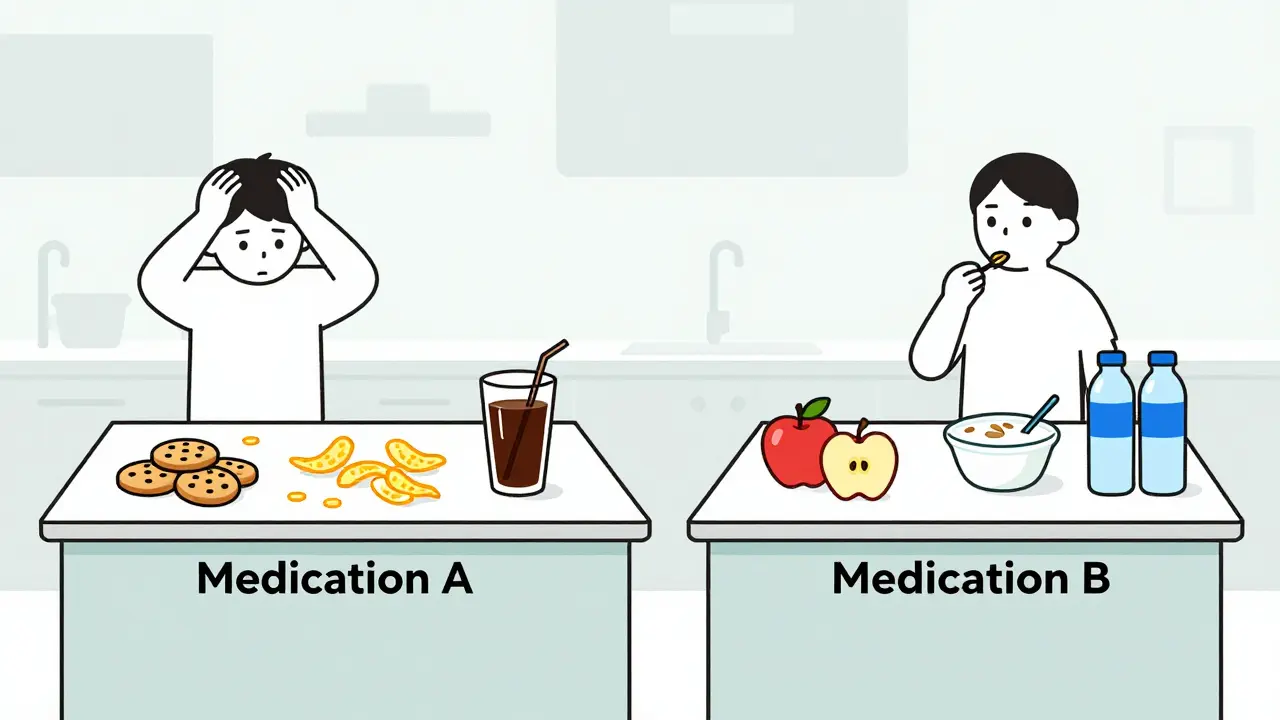
How to Manage Appetite Changes Without Stopping Your Medication
You shouldn’t quit a medication just because your appetite changed. Many of these drugs are essential for mental or physical health. The goal isn’t to stop-it’s to adapt. 1. Eat more protein and fiber. Protein keeps you full longer. Fiber slows digestion. A snack with 15-20 grams of protein (like Greek yogurt, eggs, or a protein shake) every 3-4 hours helps stabilize blood sugar and reduces sudden hunger spikes by up to 40%. Whole grains instead of white bread or pasta add fiber that extends satiety by 45 minutes per meal. 2. Change your environment. If snacks are visible, you’ll eat them. Studies show removing high-calorie, low-nutrient foods from your kitchen reduces impulsive eating by 35%. Keep fruit, nuts, and veggies front and center. Store cookies in a hard-to-reach cabinet. 3. Meal prep. When you’re hungry and tired, you grab whatever’s easiest. Planning meals twice a week cuts daily calorie intake by an average of 200 calories. That’s about 1.5 pounds a month-without dieting. 4. Practice mindful eating. Put your fork down between bites. Chew slowly. Turn off screens. People who eat mindfully reduce portion sizes by 15-20% without feeling deprived. It’s not about willpower-it’s about retraining your brain to recognize fullness. 5. Move your body. Resistance training two or three times a week builds muscle. Even a 1-2% increase in muscle mass raises your resting metabolism by 50-100 calories per day. That’s like eating one less banana daily-without trying. 6. Stay hydrated. Thirst often masquerades as hunger. Drinking a glass of water 15-20 minutes before meals helps people eat less. In one study, this simple habit reduced total calorie intake by 13%.When to Talk to Your Doctor
Weight gain or loss from medication isn’t always harmless. Rapid weight gain can raise blood pressure, worsen insulin resistance, and increase heart disease risk. Weight loss can lead to muscle wasting, fatigue, or nutrient deficiencies. The American Diabetes Association and the Endocrine Society both recommend checking your weight and waist size at the start of treatment and every three months after. If you gain more than 5% of your body weight in six months, talk to your doctor. Don’t wait until it’s 10 pounds. Your doctor might:- Switch you to a weight-neutral alternative (like switching from olanzapine to aripiprazole)
- Add metformin to counteract insulin or antipsychotic-induced weight gain
- Adjust the dose-sometimes lower doses have fewer side effects
- Refer you to a dietitian or behavioral therapist
Never stop or change your medication on your own. Tapering off antipsychotics or antidepressants too quickly can cause withdrawal, rebound symptoms, or even dangerous complications. Changes need to be slow and supervised.

New Hope: Medications Designed to Avoid Weight Gain
The pharmaceutical industry is listening. New drugs are being developed with appetite effects built into the design. Vortioxetine, approved in 2013, causes only half the weight gain of older SSRIs. Auvelity (dextromethorphan/bupropion), approved in 2022, leads to just 0.7% average weight gain-compared to 2.5% for traditional antidepressants. Even more promising is KarXT, a new antipsychotic in late-stage trials. At five weeks, users gained just 0.4 kg-versus 3.2 kg on olanzapine. That’s a game-changer for people with schizophrenia who need treatment without the burden of weight gain. Genetic testing is also emerging. Researchers have identified 12 gene variants that make some people far more likely to gain weight on certain drugs. In the next few years, doctors may be able to screen your DNA before prescribing to pick the safest option.What You Can Do Today
If you’re on a medication and notice appetite changes:- Track your weight weekly for the first three months-this is when most changes happen.
- Write down your hunger patterns: When do you feel hungriest? What do you crave?
- Start one small habit: Drink water before meals, or swap white rice for brown.
- Ask your doctor: “Is there a version of this drug that’s less likely to affect my appetite?”
- Don’t blame yourself. This isn’t about laziness or lack of discipline. It’s about chemistry.
Appetite changes from medication are real, common, and manageable. You don’t have to choose between feeling better mentally and staying healthy physically. With the right tools and support, you can do both.
Can antidepressants make you gain weight even if you eat the same amount?
Yes. Some antidepressants, especially mirtazapine and paroxetine, slow down your metabolism and increase fat storage, even if your calorie intake stays the same. Others, like bupropion, can slightly speed up metabolism. It’s not just about how much you eat-it’s how your body uses what you eat.
How long does it take for appetite changes to start after beginning a new medication?
It varies. Some people notice changes within days-especially with stimulants or antipsychotics. For antidepressants, appetite shifts often appear after 2-4 weeks. Weight gain from insulin or antipsychotics can be rapid: 4-6 kg in the first 10 weeks. The first three months are critical for monitoring.
Is weight gain from medication permanent?
Not necessarily. If you switch to a weight-neutral drug or add metformin, many people lose the extra weight over time. Behavioral changes like meal planning and exercise also help reverse gains. But the longer the weight stays on, the harder it is to lose. Early intervention matters.
Can I use weight-loss drugs while on psychiatric medication?
Sometimes, but only under medical supervision. Drugs like semaglutide (Wegovy) or phentermine can interact with psychiatric medications. Bupropion is often used safely alongside antidepressants and can help with both mood and weight. Never combine weight-loss drugs without your doctor’s approval.
Why do I crave carbs when I’m on certain meds?
Many psychiatric drugs affect serotonin. When serotonin drops, your brain seeks quick ways to boost it-carbs trigger insulin release, which helps tryptophan enter the brain and turn into serotonin. That’s why you suddenly want bread, pasta, or cookies. Choosing complex carbs (oats, quinoa, sweet potatoes) helps stabilize blood sugar and reduces the crash.
Should I avoid medication that causes appetite changes?
Not unless your doctor agrees. Many of these drugs are life-changing or life-saving. The key is to plan ahead. Ask your doctor about alternatives, start healthy habits early, and monitor your weight closely. Avoiding treatment because of fear of weight gain can lead to worse outcomes than the side effect itself.

Comments (15)