When you pick up a prescription, you might see two names on the label: one you recognize, like Lyrica, and another that looks completely different, like pregabalin. The second one is a generic drug. It’s not a copy. It’s not a lesser version. It’s the same medicine, made to the same strict standards, but it costs a fraction of the price.
What Exactly Is a Generic Drug?
A generic drug is a pharmaceutical product that contains the exact same active ingredient as a brand-name drug. It works the same way in your body, treats the same condition, and has the same risks and benefits. The only differences are in the name, shape, color, or flavor - and the price.The U.S. Food and Drug Administration (FDA) defines it clearly: a generic drug must be identical or bioequivalent to the brand-name drug in dosage form, safety, strength, route of administration, quality, performance, and intended use. That means if your doctor prescribes 10 mg of lisinopril for high blood pressure, the generic version you get from the pharmacy has the same 10 mg of lisinopril in it. No more, no less.
Generic drugs become available only after the original patent on the brand-name drug expires. Patents typically last 20 years from the date they’re filed, and during that time, only the original company can sell that drug. Once the patent runs out, other manufacturers can apply to make the same drug - but they can’t just say it’s the same. They have to prove it.
How Are Generic Drugs Approved?
The process for getting a generic drug approved is called the Abbreviated New Drug Application, or ANDA. It’s called “abbreviated” because manufacturers don’t have to repeat all the expensive animal and clinical trials that the original company did. Instead, they focus on proving one key thing: bioequivalence.Bioequivalence means the generic drug delivers the same amount of active ingredient into your bloodstream at the same rate as the brand-name drug. The FDA requires that the 90% confidence interval for two key measurements - AUC (how much drug is absorbed over time) and Cmax (the highest concentration reached) - falls between 80% and 125% of the brand-name drug. That’s a tight range. It’s not a guess. It’s science.
Manufacturers must also show that their generic drug has the same strength, dosage form (tablet, capsule, injection, etc.), and route of administration (taken by mouth, injected, applied to skin, etc.). They must meet the same quality standards, too. The FDA inspects over 3,500 generic drug manufacturing sites every year - in the U.S., India, China, and elsewhere - to make sure they follow Current Good Manufacturing Practices (cGMP). Those are the exact same rules that apply to Pfizer, Merck, or any other brand-name maker.
Why Are Generic Drugs So Much Cheaper?
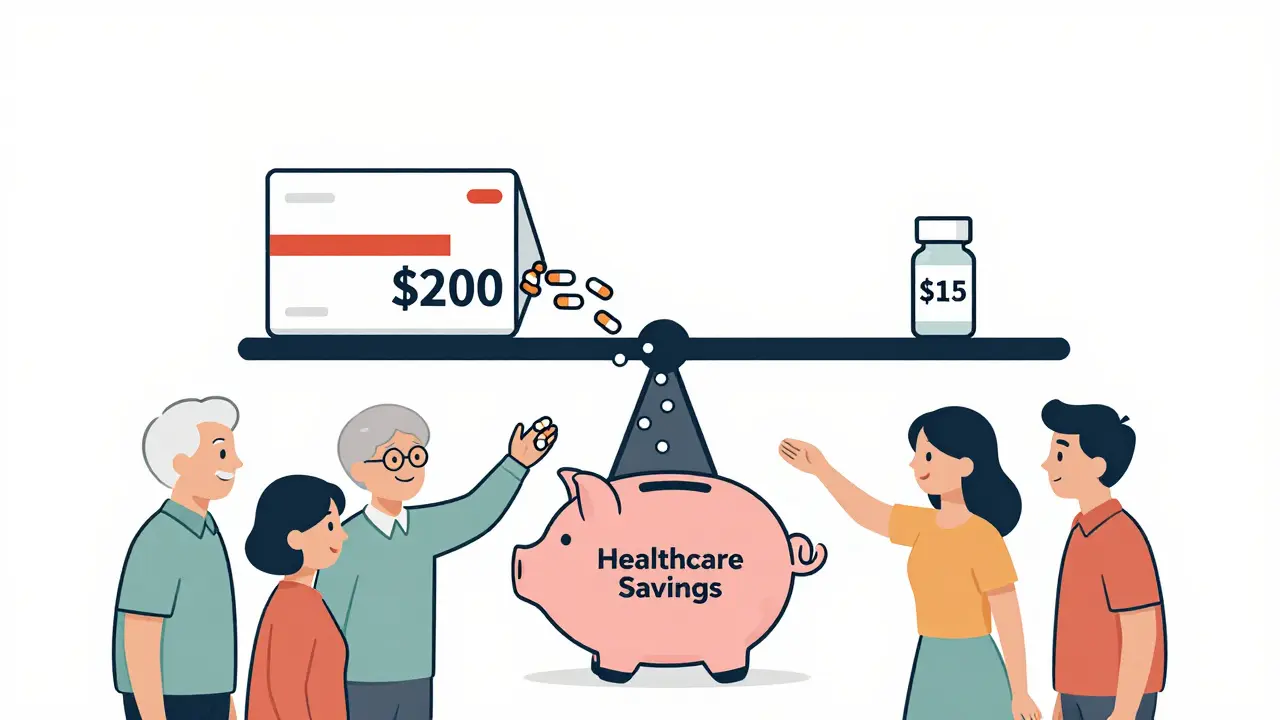
The price difference isn’t magic. It’s economics.Developing a new brand-name drug costs an average of $2.6 billion. That includes research, clinical trials, marketing, and the cost of failures - drugs that never make it to market. Generic manufacturers don’t pay that bill. They skip the R&D phase and go straight to proving bioequivalence. Their costs are mostly about manufacturing and regulatory paperwork.
As a result, generic drugs typically cost 80% to 85% less than their brand-name counterparts. In some cases, when five or more companies start making the same generic, the price drops to just 9% of the original brand price. According to the Congressional Budget Office, generic competition can slash drug prices to about 15% of the original within a year.
The impact is huge. In the U.S., generics make up 90.5% of all prescriptions filled, but they account for only 13.1% of total drug spending. Over the past decade, they’ve saved the healthcare system an estimated $2.18 trillion. That’s money that goes back into patients’ pockets, insurance premiums, and public health programs.
Are Generic Drugs Really as Safe and Effective?
Yes. And the evidence is overwhelming.The FDA doesn’t approve a generic unless it’s proven to work just like the brand. The American Medical Association, the American College of Physicians, and the Institute of Medicine have all reviewed the data and concluded that generic drugs are therapeutically equivalent to brand-name drugs.
One of the most thorough reviews came from the Institute of Medicine in 2010. They analyzed 38 clinical studies on cardiovascular drugs - things like statins, beta-blockers, and blood thinners - and found no clinically meaningful differences between generics and brand names. Patients had the same outcomes, same side effects, same success rates.
Even experts who study drug policy, like Dr. Janet Woodcock, former head of the FDA’s drug center, say plainly: “The FDA would not allow generics to be marketed unless they were therapeutically equivalent to the brand.”
There’s one exception, though. Some drugs have what’s called a “narrow therapeutic index.” That means there’s a very small range between the dose that works and the dose that causes harm. Examples include warfarin (a blood thinner), levothyroxine (for thyroid disease), and some anti-seizure medications. For these, even tiny changes in how the drug is absorbed can matter.
Doctors may recommend sticking with the same brand or generic version once you’ve started - not because generics are less effective, but because consistency helps avoid small fluctuations that could affect your health. But that doesn’t mean generics are unsafe. It just means extra care is needed.
What’s Different About Generic Drugs?
The only real differences between a generic and a brand-name drug are the inactive ingredients - things like dyes, fillers, and flavorings. These are called excipients. They don’t affect how the drug works. They’re there to make the pill look different (so it doesn’t copy the brand’s appearance), easier to swallow, or more stable on the shelf.For example, the brand-name version of omeprazole might be a red capsule with a white stripe. The generic version might be a white tablet. But both contain the same 20 mg of omeprazole. Both are tested for stability over 24 to 36 months. Both must meet the same standards for purity and potency.
The FDA allows a variation of plus or minus 5% in active ingredient content for both brand and generic drugs. That’s not a loophole - it’s standard manufacturing tolerance. Think of it like baking cookies. Two batches from the same recipe won’t be identical in size or color, but they’ll taste the same.
How Are Generic Drugs Used in Practice?
In 49 U.S. states, pharmacists can automatically swap a brand-name drug for a generic unless the doctor specifically writes “dispense as written” on the prescription. That’s called generic substitution, and it’s built into the system to save money and increase access.But patients sometimes get confused. They see a different-looking pill and think something’s wrong. That’s why pharmacists are trained to explain the difference. The Institute for Safe Medication Practices recommends that pharmacists tell patients: “This is the same medicine, just made by a different company. It’s cheaper, but just as safe and effective.”
For patients on long-term medications - like high blood pressure, diabetes, or cholesterol - switching to a generic can mean saving hundreds or even thousands of dollars a year. That’s not a small thing. For many, it’s the difference between taking the medicine and skipping doses because they can’t afford it.
The Bigger Picture: Global Trends and Challenges
The global generic drug market was worth $404.4 billion in 2022 and is expected to grow to $569.5 billion by 2028. Most of the active ingredients in generics come from India and China - about 80% of them. That’s efficient, but it also creates risks. When a single factory has quality issues, it can cause drug shortages across the U.S. and Europe.In 2022, the FDA reported a 22% increase in drug shortages, partly due to manufacturing problems at generic facilities. That’s why the agency has ramped up inspections and started requiring more detailed testing for complex generics - like inhalers, eye drops, and topical creams - where bioequivalence is harder to prove.
Another shift is happening with biologics. These are complex drugs made from living cells - like insulin, Humira, or Enbrel. They can’t be copied exactly. Instead, companies make “biosimilars,” which are highly similar but not identical. Biosimilars cost less than brand-name biologics, but only by 20% to 30%, not 80%. That’s why they’re not replacing them as quickly.
Looking ahead, 350 brand-name drugs with annual sales of $138 billion are set to lose patent protection between 2023 and 2027. That means a wave of new generics is coming. More competition. Lower prices. More access.
Final Thoughts: Why It Matters
Generic drugs aren’t a compromise. They’re a solution. They’re how millions of people get the medicines they need without going broke. They’re how healthcare systems stay sustainable. They’re how patients with chronic conditions can stick to their treatment plans.There’s no reason to fear them. The science is clear. The regulations are strict. The results are proven. If your doctor offers you a generic, it’s not because they’re cutting corners. It’s because they care - about your health, and your wallet.
Are generic drugs as effective as brand-name drugs?
Yes. Generic drugs must meet the same FDA standards as brand-name drugs. They contain the same active ingredient, in the same strength, and deliver it to your body at the same rate. Studies have shown no meaningful difference in effectiveness for most medications. The FDA requires proof of bioequivalence before approving any generic.
Why do generic drugs look different from brand-name drugs?
By law, generic drugs can’t look exactly like the brand-name version - that’s to avoid trademark infringement. So they may be a different color, shape, or size. But the active ingredient, dosage, and effectiveness are identical. The differences are only in inactive ingredients like dyes or fillers, which don’t affect how the drug works.
Can I trust generic drugs made in other countries?
Yes. The FDA inspects all manufacturing facilities - whether they’re in the U.S., India, China, or elsewhere - using the same strict standards. Over 3,500 inspections are done each year. If a facility doesn’t meet cGMP (Current Good Manufacturing Practices), the FDA blocks the product from entering the U.S. market.
Are there any drugs where I should avoid generics?
For most drugs, generics are perfectly safe. But for medications with a narrow therapeutic index - like warfarin, levothyroxine, or certain seizure drugs - even small changes in absorption can matter. In these cases, doctors may recommend staying on the same version (brand or generic) once you’ve started. This isn’t because generics are unsafe - it’s about consistency and minimizing risk.
Why are generic drugs so much cheaper?
Generic manufacturers don’t have to pay for the original research, clinical trials, or marketing that brand-name companies do. Those costs can exceed $2.6 billion per drug. Generics only need to prove bioequivalence, which is far less expensive. That’s why they typically cost 80-85% less than brand-name drugs.
Do generic drugs have the same side effects?
Yes. Since they contain the same active ingredient and work the same way in the body, generic drugs have the same side effect profile as their brand-name counterparts. Any differences in side effects are usually due to individual reactions to inactive ingredients, which are rare and usually mild.
Can pharmacists switch my brand-name drug to a generic without asking me?
In 49 U.S. states, yes - unless your doctor writes “dispense as written” on the prescription. Pharmacists are trained to substitute generics to save money, and they’re required to inform you if they do. You always have the right to ask for the brand-name version, but you may pay more.


Comments (12)
Man, I work in pharma back in India and let me tell you - we churn out generics like chai at a dhaba. Same active ingredient, same results. People here think we're cutting corners, but nah. We're just not charging for someone else's R&D bill. FDA checks us harder than my mom checks my homework.
OMG I tried generics once and my anxiety got WORSE. Like, I swear I felt like my brain was swimming in molasses. I went back to the brand and boom - instant peace. So no, not all generics are equal. Someone’s gotta speak up for the people who actually feel the difference.
It’s important to recognize that for most people, generics are a lifeline. But Jacqueline’s experience isn’t invalid either - for drugs with narrow therapeutic windows, consistency matters. It’s not about distrust, it’s about personal physiology. Doctors should have more flexibility to tailor this, not just default to savings.
You think that’s bad? I’ve seen generics made in factories where the workers wear flip-flops and the QA guy is the guy who cleans the toilets. The FDA doesn’t inspect every batch. They inspect paperwork. Big difference. Don’t be fooled by the shiny label.
Bro, in India we make 70% of the world’s generics. We don’t cut corners - we cut costs. The science is solid. I’ve seen my uncle take generic blood pressure meds for 12 years. Still alive. Still working. Still paying for groceries. That’s the real win.
How delightfully quaint that we’ve reduced human health to a spreadsheet equation. One might assume that the sanctity of pharmaceutical integrity is merely an impediment to fiscal efficiency. How tragic that we’ve elevated cost-cutting to the status of moral virtue, while dismissing the nuanced, irreplaceable art of medical precision as mere ‘branding.’
Let’s be real - generics saved my dad’s life. He’s on three of them. Without them, he’d be choosing between insulin and rent. I get the fear, but don’t let fear make you forget the people who can’t afford the fancy version. We’re not talking about candy here - we’re talking about survival.
My pharmacist switched my generic without telling me, and I didn’t notice a thing. But I did notice my co-pay dropped from $85 to $8. That’s not magic, that’s common sense. Why pay more for the same thing? Unless you’re allergic to the dye, it’s fine.
Generic drugs are the unsung heroes of modern medicine nobody talks about until they’re out of stock then everyone’s screaming. Meanwhile the same people who hate generics are the ones who cry when their insurance hikes premiums because they insisted on the brand. Wake up people
So let me get this straight - you’re telling me the same FDA that approved the opioid crisis is now our guardian angel for pill color and shape? I’ll take my brand-name, thank you very much. At least I know who to blame when it doesn’t work.
Just had my first generic switch - took the pill, went for a walk, felt totally normal. No brain fog, no panic. Just saved $90. 🙌 If you’re scared, ask your doc. But don’t let fear stop you from saving your wallet. You’re not a guinea pig - you’re a smart consumer.
My cousin works at a generic plant in Hyderabad. They have ISO-certified labs, robotic fillers, and FDA auditors coming every quarter. The real problem? Supply chains. When one factory in China gets shut down, the whole world feels it. Not because generics are bad - because we’re too dependent on a few hubs.