Generic Medication Savings: How to Save Big Without Sacrificing Quality
When you hear generic medication savings, the cost reduction from using FDA-approved versions of brand-name drugs without changing effectiveness. Also known as generic drugs, they work the same way, have the same active ingredients, and are held to the same safety standards as their brand-name counterparts. Yet many people still pay more than they need to because they’re unsure if generics are truly equal. The truth? They are. The FDA requires them to be bioequivalent—meaning they deliver the same amount of medicine into your bloodstream at the same rate. You’re not getting a lesser product. You’re getting the same result for 80% less money.
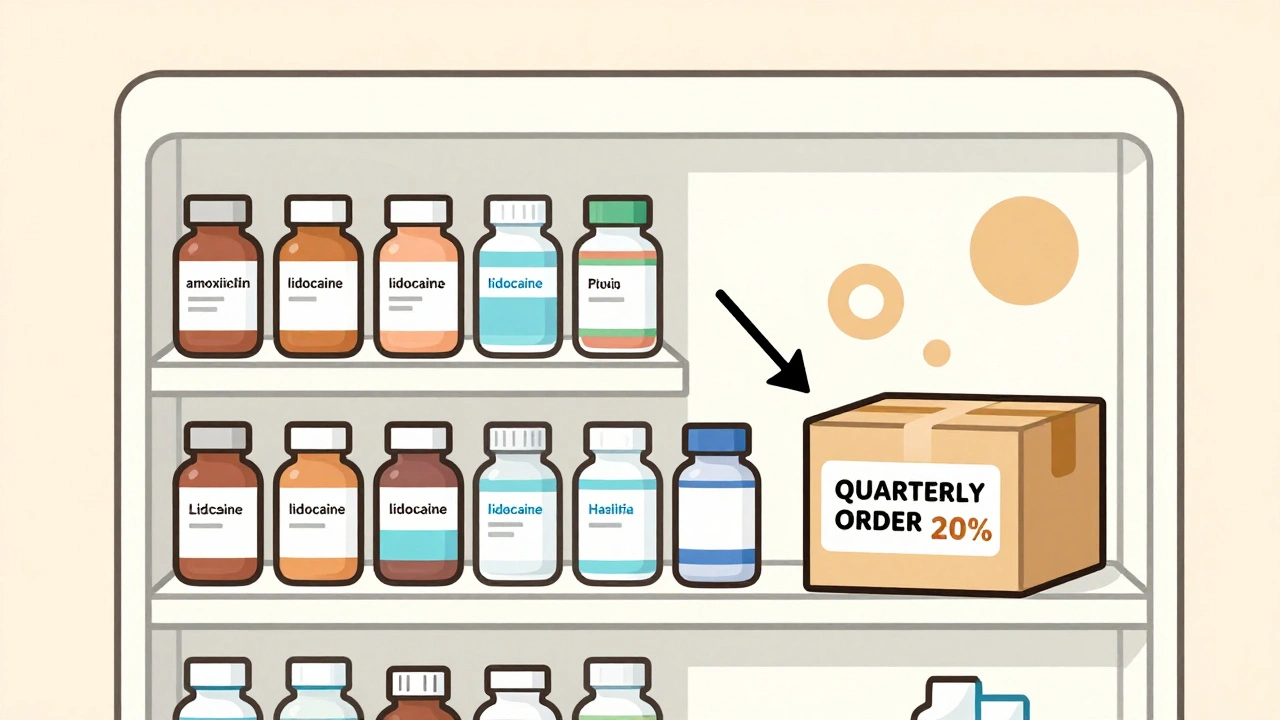
This isn’t just about saving a few dollars on a monthly prescription. It’s about making long-term treatment possible. People on statins for cholesterol, thyroid meds like levothyroxine, or even blood pressure drugs like isosorbide mononitrate often take these pills daily for years. That adds up fast. With generic drugs, FDA-approved versions of brand-name medications that contain the same active ingredients and meet identical standards, a $300 brand-name pill can drop to $10. That’s life-changing for families on fixed incomes or those without good insurance. And it’s not just about price. When meds are cheaper, people take them as prescribed. Studies show adherence improves by up to 30% when patients switch to generics. Better adherence means fewer hospital visits, fewer complications, and better health outcomes.
Some worry about differences in fillers or inactive ingredients. Sure, generics might look different—different color, shape, or coating—but those don’t affect how the medicine works. The active ingredient? Identical. The manufacturing? Held to the same strict rules as brand-name factories. In fact, many brand-name companies make their own generics under a different label. The real difference? Marketing. Brand names spend millions on ads. Generics don’t. That’s where the savings come from.
Not all drugs have generics yet. Newer biologics like Humira or Enbrel still carry high prices because patent protections delay competition. But for most common conditions—high blood pressure, diabetes, depression, acid reflux—there’s a generic option that works just as well. Pharmacists recommend them not because they’re cheap, but because they’re smart. When your pharmacist suggests switching to a generic, they’re not trying to cut corners. They’re helping you stay healthy without breaking the bank.
And it’s not just about what’s on the label. Legal battles over patents, like those under the Hatch-Waxman Act, shape when generics enter the market. Court cases have forced big drugmakers to stop gaming the system with minor reformulations just to delay competition. That’s why more generics are hitting shelves now than ever before. You’re not just saving money—you’re benefiting from a system designed to make medicine affordable.
Below, you’ll find real-world examples of how people save thousands a year by choosing generics. You’ll learn how to spot when a generic is available, how to talk to your doctor about switching, and which brand-name drugs still cost too much even with a generic alternative. These aren’t theoretical savings. They’re lived experiences—from someone managing cholesterol with ezetimibe instead of a pricier brand, to a parent switching their child’s ADHD med to cut monthly costs in half. This is the practical side of medication savings. No fluff. Just what works.
- December 2, 2025
- Comments 11
- Medications and Supplements