Large-Scale Pharmaceutical Procurement: How Hospitals and Pharmacies Source Medicines Safely
When you think about how your prescription gets to the pharmacy shelf, you probably don’t picture warehouses, contracts, or bidding wars—but that’s where large-scale pharmaceutical procurement, the systematic buying of medicines in bulk by hospitals, health systems, and pharmacy chains. Also known as bulk drug procurement, it’s the quiet engine behind every pill, injection, and inhaler you use. This isn’t just about buying cheap—it’s about making sure the right drugs arrive on time, at the right price, and without contamination or counterfeits.
Behind every hospital’s drug inventory is a team managing pharmaceutical supply chain, the network of manufacturers, distributors, regulators, and logistics providers that move drugs from labs to patients. It’s a high-stakes operation. One bad batch of antibiotics or a delay in insulin delivery can cost lives. That’s why procurement isn’t just a finance task—it’s a clinical safety issue. The same rules that keep your meds safe at home—checking labels, avoiding expired drugs, knowing what’s in your bottle—apply on a massive scale, but with more layers of oversight. generic drug procurement, the process of buying FDA-approved versions of brand-name drugs in bulk to cut costs makes up over 90% of prescriptions in the U.S., but getting those generics right means verifying manufacturers, checking bioequivalence, and auditing production sites—even overseas.
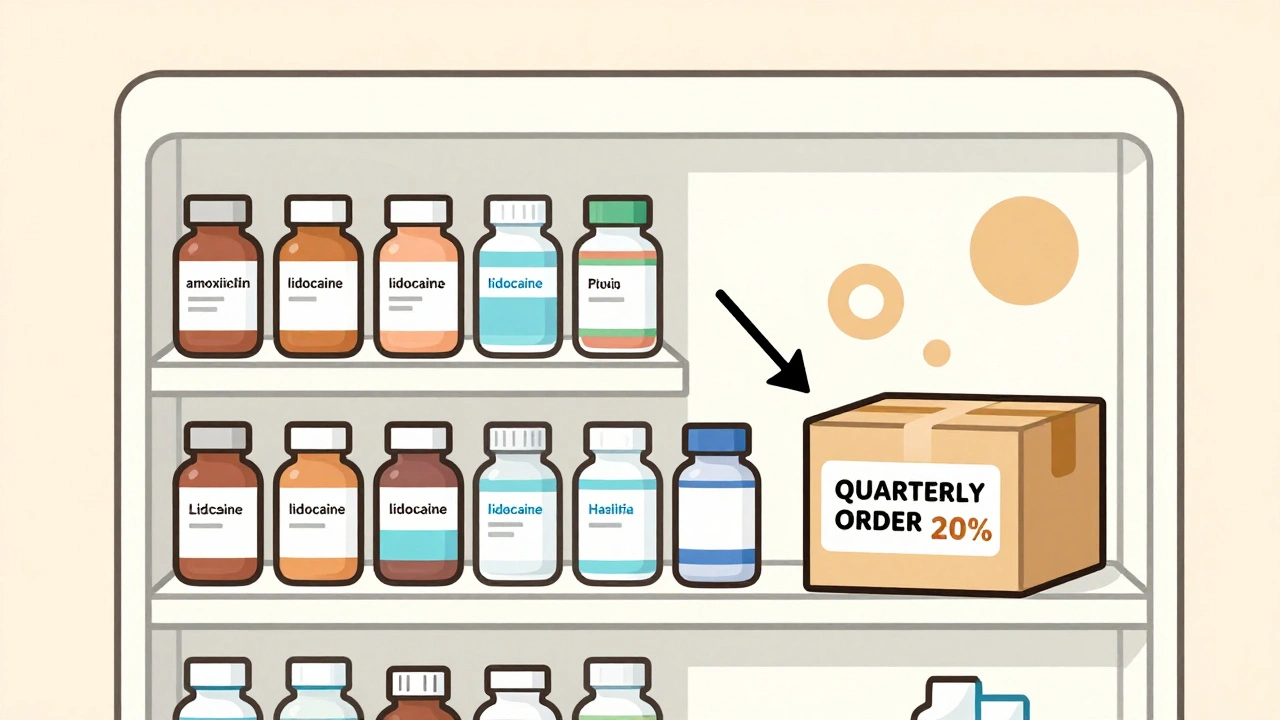
What you won’t see on the label is how much negotiation goes into this. Hospitals don’t just order from the first vendor. They run RFPs, compare pricing across states, bundle drugs to get volume discounts, and track inventory in real time to avoid overstocking or shortages. And it’s not just about price. A single drug recall can ripple through a whole system, which is why procurement teams now demand traceability, batch numbers, and digital records—something you’ll see reflected in posts about sterile manufacturing, biosimilars, and patent law. This is where the rubber meets the road: when a hospital buys 10,000 doses of a statin or a biologic, they’re not just spending money—they’re betting on safety, consistency, and reliability.
And here’s the thing: what works for a big hospital doesn’t always work for a small pharmacy. But the same principles apply—know your supplier, verify your source, and never assume. That’s why the posts here cover everything from how patent lawsuits affect drug prices to why sterile manufacturing standards matter even for pills you take at home. Whether you’re a pharmacist managing inventory, a hospital administrator watching budgets, or just someone wondering why your meds cost what they do—this collection gives you the real picture behind the curtain. You’ll find the facts that don’t make headlines, but keep you alive.
- December 2, 2025
- Comments 11
- Medications and Supplements