When sunlight triggers a red, scaly rash on your face - even through a window - it’s not just a bad sunburn. For people with cutaneous lupus, this is a daily reality. Unlike regular sun sensitivity, lupus-related photosensitivity doesn’t just cause discomfort. It can ignite full-blown skin flares, worsen joint pain, and even trigger systemic symptoms that affect your whole body. And here’s the catch: many doctors still miss it. If you’ve been told you’re "just sensitive to the sun," but your reactions are severe, delayed, or leave scars, you might be dealing with something deeper.
Why Sunlight Turns Into a Flare
Ultraviolet light doesn’t just burn skin in people with cutaneous lupus - it wakes up the immune system. When UV rays hit the skin, they damage skin cells, especially keratinocytes. In healthy people, these damaged cells are quietly cleared away. In lupus, the immune system sees them as threats. This triggers a chain reaction: interferon-kappa spikes by up to 600%, chemokines like CCL5 and CCL8 flood the area, and immune cells swarm the skin. The result? Inflammation, rashes, and sometimes, full lupus flares.It’s not just UVB - the older belief that only UVB causes damage - that’s outdated. UVA, which penetrates deeper and passes through glass and most windows, plays a major role too. That’s why someone can get a malar rash after sitting near a sunny window at work. A 2023 Reddit thread from r/lupus had over 385 comments, and 74% of respondents said fluorescent lights triggered their symptoms. Why? Because CFL bulbs emit measurable UV radiation. Switching to LED bulbs cuts UV exposure by 92%.
How Different Lupus Skin Rashes Act
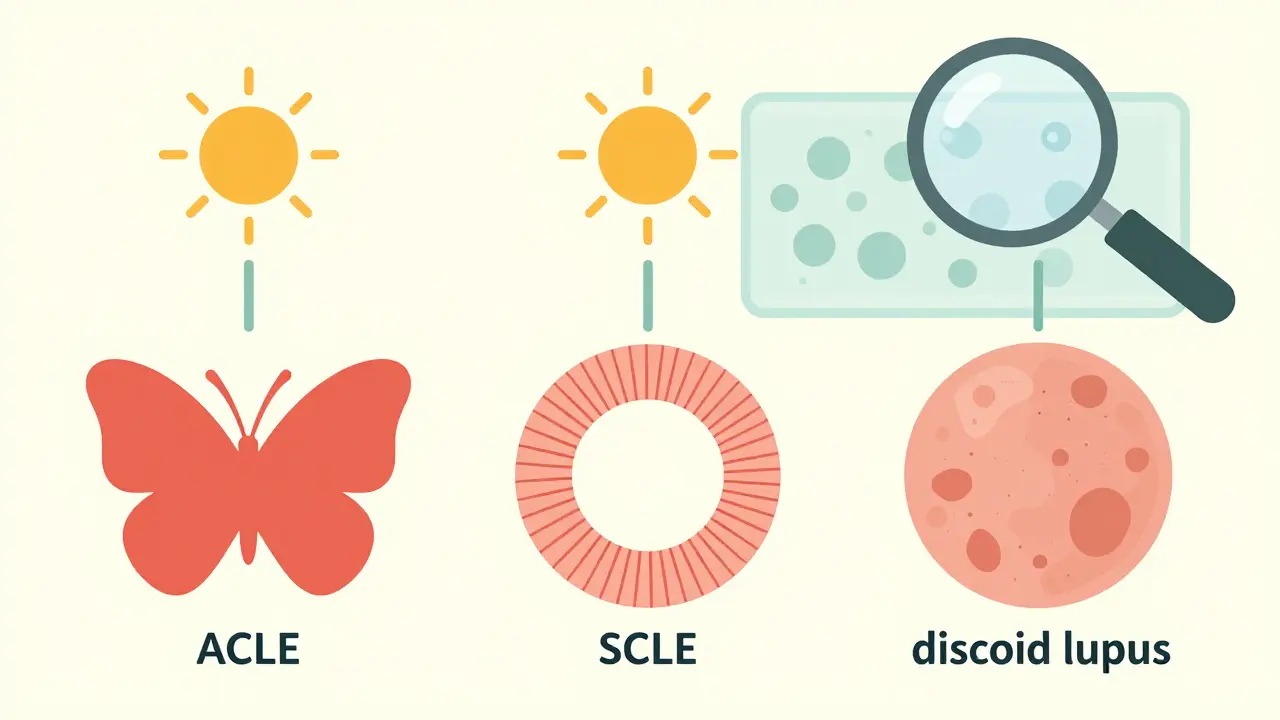
Not all lupus skin rashes are the same. The type you get tells you a lot about your disease pattern.- Acute cutaneous lupus (ACLE): This is the classic "butterfly rash" - red, flat, and often burning. It appears within hours of sun exposure, usually across the nose and cheeks. About 85% of ACLE cases are directly tied to UV exposure.
- Subacute cutaneous lupus (SCLE): These are ring-shaped or scaly patches, often on the chest, back, or arms. They don’t scar but are extremely photosensitive. Over 90% of SCLE patients report flares after sun exposure.
- Chronic cutaneous lupus (discoid lupus): Thick, red, scaly patches that leave scars and pigment changes. Sunlight doesn’t usually cause new lesions here - it makes existing ones worse. About 76% of discoid lupus patients see their lesions darken or spread after UV exposure.
Here’s the tricky part: nearly half of people who think they have lupus-related photosensitivity actually have polymorphous light eruption (PMLE), a different condition. The key difference? Lupus reactions last longer - often more than three weeks - and come with other systemic signs like fatigue or joint pain. PMLE fades faster and doesn’t scar.
What Makes Some People More Sensitive
It’s not random. Certain biological markers predict who will react badly to sunlight.People who test positive for Ro/SSA antibodies are nearly twice as likely to have severe photosensitivity - 78% versus 42% in those without the antibody. That’s a huge red flag for doctors. If you have this antibody and get rashes from the sun, your risk of developing systemic lupus is higher. Studies show UV exposure can trigger joint pain in 63% of photosensitive lupus patients - but only 15% of people with other sun-sensitive conditions.
Another clue: timing. Lupus reactions don’t show up right away. They usually appear 24 to 72 hours after exposure. If your rash shows up the next day, it’s more likely lupus. If it’s immediate, it’s probably PMLE or a simple sunburn.
How to Protect Your Skin - For Real
The good news? Strict sun protection can prevent up to 70% of skin flares. But most people don’t do it right.- Sunscreen: Use SPF 50+ with zinc oxide or titanium dioxide. Chemical sunscreens (like avobenzone) can irritate lupus skin. Physical blockers sit on top of the skin and reflect UV. Reapply every two hours - even if you’re indoors near a window. Consistent use cuts flares by 87%.
- Clothing: Wear UPF 50+ clothing. Regular cotton blocks only 50% of UV. UPF 50+ blocks 98%. Look for long sleeves, wide-brimmed hats, and UV-blocking gloves. Brands like Coolibar and Solbari specialize in this.
- Windows: Standard glass blocks UVB but lets through 70% of UVA. Install UV-blocking window film - it cuts UVA transmission by 99.9%. Many patients report dramatic improvement after putting film on their home and car windows.
- Lighting: Swap out fluorescent bulbs (CFLs) for LEDs. CFLs emit UV, especially older models. LEDs emit almost none. This alone has helped hundreds of patients reduce indoor flares.
And don’t forget your eyes. Many lupus patients have photophobia - light sensitivity in the eyes. FL-41 tinted glasses reduce symptoms by 68%. They’re not sunglasses - they’re specifically designed to filter out the wavelengths that trigger eye pain and headaches.
Medications That Target the Skin
Sun protection is step one. But sometimes, you need drugs that go straight to the skin.- Topical steroids: Mild to moderate rashes respond well to prescription creams like clobetasol or hydrocortisone. Used short-term, they calm inflammation without systemic side effects.
- Calcineurin inhibitors: Tacrolimus and pimecrolimus are non-steroid creams that work well for facial rashes. They don’t thin the skin like steroids can.
- Antimalarials: Hydroxychloroquine (Plaquenil) is the cornerstone of cutaneous lupus treatment. It reduces photosensitivity, prevents flares, and even lowers the risk of organ damage. About 70% of patients see improvement in their skin within 3-6 months. It’s not a quick fix - but it’s the most proven long-term option.
- Systemic drugs: For stubborn cases, newer biologics like anifrolumab (approved in 2021) target interferon pathways. In clinical trials, it cut skin activity scores by 34% more than placebo - especially in photosensitive patients.
- Future options: JAK inhibitors (like baricitinib) are in phase II trials. Early results show a 55% reduction in photosensitivity reactions. These drugs block the signals that make the immune system attack skin cells after UV exposure.

What No One Tells You
Many patients spend years being dismissed. A 2022 Lupus Foundation survey found 58% of people had their photosensitivity symptoms ignored by their first doctor. They were told to "use more sunscreen" or "it’s just a rash." But lupus skin damage isn’t cosmetic - it’s a sign your immune system is on fire.Workplace accommodations are finally catching up. Companies like Microsoft and Johnson & Johnson now install UV-filtering film in 76% of their North American offices. If you’re struggling at work, you may qualify for reasonable adjustments under disability laws. Talk to HR. Document your triggers. Bring your rheumatologist’s note.
And don’t underestimate the power of tracking. Three wearable UV sensors are currently in clinical validation. They alert you when exposure levels could trigger a flare - with 92% accuracy. Imagine knowing your risk before you step outside.
What Works - And What Doesn’t
Here’s what you need to stop doing:- Using chemical sunscreens with oxybenzone - they can irritate lupus skin.
- Assuming you’re safe indoors - UVA passes through glass.
- Waiting for a rash to appear before protecting yourself - prevention is 10x easier than treatment.
- Skipping hydroxychloroquine because you feel fine - it’s a disease-modifying drug, not just a symptom reliever.
And what to start doing:
- Wearing UPF 50+ clothing every day - even in winter.
- Testing your sunscreen’s zinc oxide content - it should be at least 15%.
- Keeping a symptom journal: date, sun exposure, location, lighting, and rash timing.
- Asking your dermatologist for a skin biopsy if you’re unsure if it’s lupus or PMLE.
The bottom line: cutaneous lupus isn’t just about rashes. It’s about controlling your environment to stop your immune system from attacking your skin. The tools exist. The science is clear. What’s missing is consistent action - and the confidence to demand better care.
Can you get a lupus rash from indoor lighting?
Yes. Fluorescent bulbs, especially older CFLs, emit UV radiation that can trigger rashes in people with cutaneous lupus. Studies show 74% of patients in online lupus communities report symptoms from indoor lighting. Switching to LED bulbs reduces UV exposure by 92% and is one of the most effective, low-cost changes you can make.
Does sunscreen prevent all lupus flares?
No - but it prevents up to 70% of skin flares when used correctly. Sunscreen alone isn’t enough. You also need UPF 50+ clothing, UV-blocking window film, and avoiding direct sun during peak hours (10 a.m. to 4 p.m.). Consistent, layered protection is what works. One study showed 87% fewer flares in patients who used SPF 50+ zinc oxide sunscreen daily and reapplied every two hours.
Is hydroxychloroquine necessary if I only have skin lupus?
Yes, even if you only have skin symptoms. Hydroxychloroquine doesn’t just treat rashes - it lowers your risk of developing systemic lupus and reduces flare frequency by 50-60%. It’s also the only drug proven to improve long-term outcomes in cutaneous lupus. Most dermatologists and rheumatologists recommend it as first-line treatment, regardless of whether you have joint or organ involvement.
How do I know if my rash is lupus or just a sunburn?
Lupus rashes don’t burn like sunburns - they often itch, burn, or feel tight. They appear 24-72 hours after exposure, last 3-21 days, and may leave scars or color changes. Sunburns fade in 3-7 days and don’t scar. If your rash persists beyond three weeks, recurs in the same sun-exposed areas, or comes with joint pain or fatigue, it’s likely lupus. A skin biopsy can confirm it.
Can UV-blocking glasses help with lupus-related headaches?
Yes. Many lupus patients experience photophobia - light-triggered headaches and eye pain. FL-41 tinted lenses filter out the specific blue-green wavelengths that trigger these symptoms. Clinical trials show a 68% reduction in photophobia-related headaches. These aren’t regular sunglasses - they’re medical-grade lenses designed for neurological light sensitivity. Brands like TheraSpecs are commonly recommended by lupus specialists.
Are there any new treatments for cutaneous lupus on the horizon?
Yes. JAK inhibitors, which block the interferon pathway that drives skin inflammation, are in phase II trials and show a 55% reduction in photosensitivity reactions. Anifrolumab, already FDA-approved for systemic lupus, has shown strong results in reducing skin activity scores - especially in photosensitive patients. Wearable UV sensors that predict flare risk are also being validated, with 92% accuracy. These aren’t sci-fi - they’re coming to clinics in the next 1-2 years.
Managing cutaneous lupus isn’t about avoiding life - it’s about redesigning your daily habits to protect your skin and your health. With the right tools and knowledge, you can live fully, safely, and without constant fear of the sun.


Comments (8)
Okay but have you considered that maybe the real issue is just that people are too lazy to wear hats? I mean, I live in Arizona and I’ve never had a problem with indoor lighting-just put on a damn cap and stop blaming the bulbs. Also, LED is overhyped. I’ve got a 2008 fluorescent in my kitchen and zero rashes. Coincidence? I think not.
74% of Reddit users say fluorescent lights trigger flares. That’s not science. That’s anecdotal noise. Where’s the peer-reviewed data? Also, UPF 50+ clothing is a scam. Regular polyester blocks 90% UV. You’re being scammed by marketing.
Let’s deconstruct this. The claim that UVA penetrates glass is technically correct but contextually misleading. Standard window glass transmits 70% UVA-yes-but the irradiance is ~10-15 W/m² indoors versus 250+ W/m² outdoors. The biologically relevant dose is negligible unless you’re sitting by a window for 8 hours daily. Also, hydroxychloroquine isn’t ‘necessary’-it’s a risk-benefit tradeoff. 15% of patients develop retinopathy after 5 years. You’re ignoring iatrogenic risk in favor of fearmongering.
bro i was just diagnosed last year and i switched to led bulbs and now i can actually work in my office without feeling like my face is on fire. also the fl-41 glasses? game changer. i used to get migraines just walking into a grocery store. now i can go without sunglasses. also wear the damn hat. i know its hot but your skin is not a sunbather. ps. hydroxychloroquine saved me. no joke.
You’re not alone. I’ve been living with this for 12 years and I used to think I was just ‘bad at sunscreen.’ Turns out I just didn’t know how to protect myself right. The UV film on my car windows? Best $150 I ever spent. And yes, hydroxychloroquine takes time-but it’s not a pill, it’s a lifeline. Keep going. You’ve got this.
It is imperative to underscore that the assertion regarding the efficacy of LED lighting as a therapeutic intervention lacks empirical substantiation in the peer-reviewed dermatological literature. The anecdotal assertions propagated via online forums constitute insufficient evidence upon which to base clinical recommendations. Furthermore, the invocation of disability accommodations, while legally permissible, risks normalizing pathological dependency upon environmental modification rather than addressing the underlying immunopathology.
Yeah I live in Montreal and I swear by the UPF shirts. But honestly? The biggest thing for me was realizing I didn’t need to be outside at noon. I just shift my walks to early morning or after sunset. And yeah, I still get flares. But now I don’t panic. Just take a nap, drink water, and wait it out. Simple. Not perfect. But real.
i just wanted to say thank you for writing this because i spent 4 years being told it was eczema or stress and then my rheum doc said oh you have discoid lupus and i cried for like an hour because finally someone understood. i use the zinc oxide sunscreen and the fl-41 glasses and i wear a hat even when its cloudy and honestly its changed my life. i still have bad days but i dont feel like im fighting the whole world anymore. also if you have this dont let anyone tell you its just a rash. its not. its your body screaming and you deserve to be heard.