Keeping emergency medications like epinephrine, naloxone, or heart medications both accessible and secure isn’t just a good idea-it’s a life-or-death balance. Too locked up, and you risk delay during a crisis. Too loose, and you risk accidental overdose, theft, or a child getting into it. The truth is, there’s no single perfect solution. What works for a hospital ward won’t work for a home, a school, or an ambulance. But the principles are the same: know your meds, know your risks, and build a system that fits your real-world situation.
Know What You’re Storing
Not all emergency meds are created equal. Epinephrine auto-injectors (like EpiPens) need to stay between 20°C and 25°C (68°F-77°F). If they get too hot or too cold, they lose potency. Naloxone (Narcan) is more forgiving but still shouldn’t freeze. Insulin for diabetic emergencies? That one needs refrigeration-until it’s in use. And if you’re storing controlled substances like opioids for severe pain, federal rules require them to be locked in a substantially built cabinet with a lock, separate from other meds.Check the label. Check the manufacturer’s instructions. And don’t assume every pharmacy gives you clear storage info-only 43% of prescription labels in 2022 included full storage details, according to the FDA. If in doubt, call the manufacturer or your pharmacist. A wrong temperature can turn a lifesaver into a useless pill.
Home Storage: Lock It, But Not Too Tight
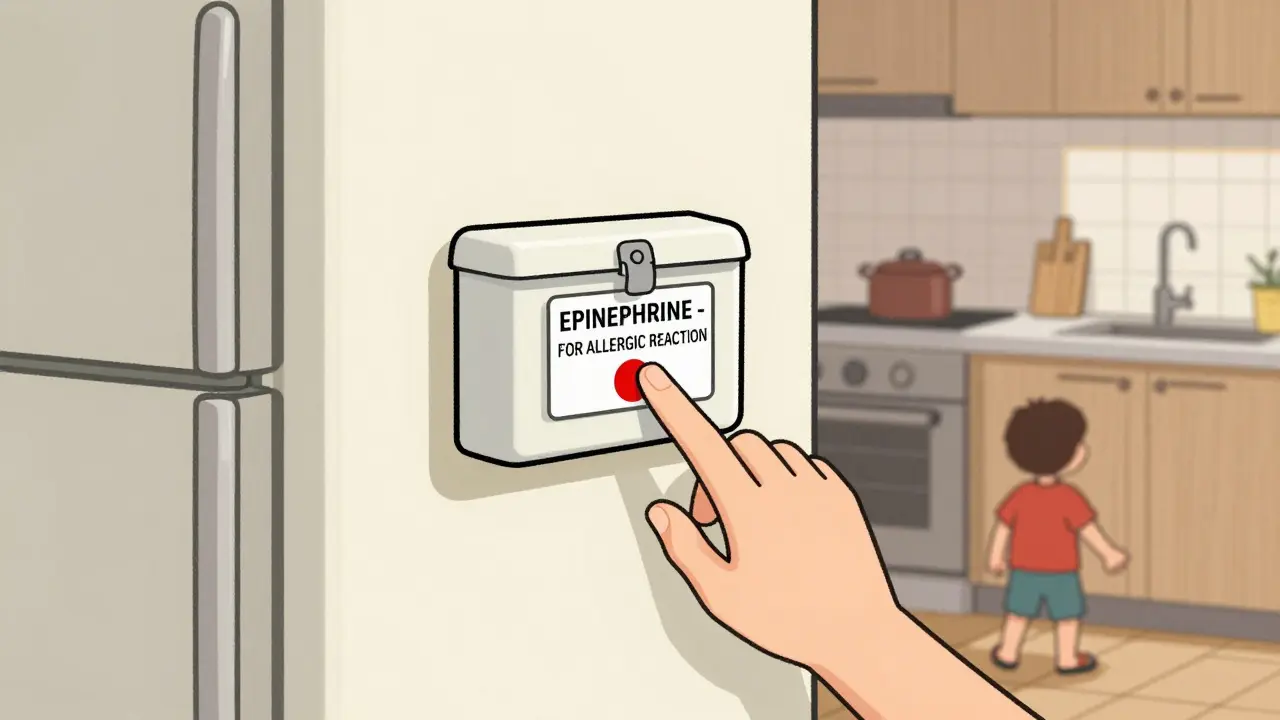
In a home, your biggest risks are kids, pets, or visitors who don’t know what they’re handling. The EPA recommends locked cabinets, closets, or safes. But here’s the catch: if it’s locked behind three keys and a code, and you’re the only one who can open it, you’ve created a new danger.Think about where you live. If you have young children, keep emergency meds in a high cabinet with a childproof latch-not a toy box, not a drawer. If you or someone in your home has a condition like severe allergies or opioid overdose risk, keep the med right next to the person who needs it-like in a wallet, purse, or bedside box. Just make sure it’s labeled clearly: “EPINEPHRINE - FOR ALLERGIC REACTION - DO NOT USE UNLESS SYMPTOMS PRESENT.”
Medicine safes are cheap now-under $50 for a basic one with a keypad or fingerprint lock. You don’t need a vault. You need something sturdy enough that a toddler can’t open it, but fast enough that you can grab it in 3 seconds. Test it. Have someone else try to open it blindfolded. If it takes more than 5 seconds, it’s too slow.
Workplace & Caregiver Settings
Schools, daycare centers, and nursing homes have different rules. The CDC and Child Health Connection say emergency meds for allergies or seizures don’t need to be locked if they’re kept in a location staff can reach instantly-like a locked box on the wall next to the nurse’s station, or a clearly marked drawer in the first-aid kit. But routine meds? Those go in locked cabinets.Key point: If a child has an epinephrine prescription, the school must have a plan. That means staff are trained, the med is labeled, and someone always knows where it is. No more “I didn’t know it was in the fridge” or “I thought it was with the teacher.” Document it. Practice drills. The Joint Commission says 17 sentinel events between 2021 and 2023 happened because someone couldn’t find the med when seconds counted.

EMS and Clinical Settings: Speed Is Everything
In ambulances or ERs, the rules get more technical. Medications must be stored in lockable cabinets that stay secure when not in use-but keys or codes must be with trained staff only. In hospitals, code carts often have tamper-evident seals. If someone opens it, you’ll know. That’s the goal: prevent theft, but never delay care.Temperature matters here too. EMS providers in 32% of agencies reported meds going out of range during winter or summer heat. That’s why portable monitors like TempTraq are becoming common. They beep if the box hits above 30°C or below 2°C. No more guessing. Just a red light and a quick fix.
And here’s the hard truth: 17.3% of EMS crews reported delays in 2022 because the med was locked too tightly. One paramedic in Oregon told a national survey, “We had to wait 90 seconds for the supervisor to unlock the cabinet while the patient was coding.” That’s not security-that’s negligence. The solution? Dual access: one key for the lead medic, one for the backup. Or a code shared among two trained people. No single point of failure.
Transport and Travel
Traveling with emergency meds? Don’t pack them in checked luggage. Heat, cold, pressure-they’ll wreck the drug. Keep them in your carry-on, in a small insulated pouch with a cool pack if needed. For epinephrine or insulin, use a travel cooler that maintains 2°C-8°C. Many pharmacies sell these for under $20.And never, ever leave meds in a car. Even in winter, a car can hit 40°C (104°F) in sunlight. That’s the threshold where many drugs start breaking down. The NVERS guidelines say above 40°C is “excessive heat.” Don’t risk it.

Disposal: Don’t Flush, Don’t Trash
Expired or unused meds? Don’t throw them in the trash or flush them. The EPA and FDA both warn against this-it contaminates water and invites misuse. Instead, use a drug take-back program. Most pharmacies, hospitals, or police stations have drop boxes. In the UK, you can return them to any pharmacy for safe disposal.If there’s no take-back nearby, mix pills with coffee grounds or cat litter, put them in a sealed container, and throw them in the trash. That makes them unappealing and unrecognizable. For injectables like EpiPens, use a sharps container. Many pharmacies give them out free.
Training and Practice
You can have the best storage system in the world, but if no one knows how to use it, it’s useless. A 2023 study found that after two 2-hour training sessions, 85% of healthcare workers could correctly access, identify, and use emergency meds under pressure.Do this: Once a month, run a 30-second drill. “Your child is having an allergic reaction. Where’s the EpiPen?” Time how long it takes to find it. Do it with visitors. Do it with kids who are old enough to understand. Make it routine. Like fire drills.
And document it. Keep a log: “EpiPen checked on Feb 3, 2026. Exp. date: July 2026. Stored in red box on kitchen wall.”
The Bottom Line
There’s no magic box. No one-size-fits-all. But there are smart habits:- Know your meds’ temperature needs
- Lock them, but not so tight that you can’t reach them in 5 seconds
- Label everything clearly
- Train everyone who might need to use them
- Check expiration dates every 3 months
- Dispose of old meds properly
Emergency meds aren’t just pills. They’re your insurance against the unexpected. Treat them like a fire extinguisher: ready, visible, and tested. Not hidden. Not forgotten. Not locked away forever.
Can I keep emergency medication in the fridge?
Only if the medication specifically requires refrigeration-like insulin or some forms of epinephrine. Most emergency meds, including naloxone and EpiPens, are meant for room temperature (20°C-25°C). Storing them in the fridge can damage the drug or cause condensation that ruins the packaging. Always check the label or ask your pharmacist.
What’s the best way to store naloxone at home?
Keep it in a small, labeled container in a place that’s easy to reach-like a bedside drawer, kitchen counter (if kids aren’t around), or a locked cabinet with a quick-access code. Naloxone doesn’t need refrigeration. Avoid bathrooms (too humid) and cars (too hot). Test your system: can your partner find it in under 10 seconds?
Is it legal to keep opioids at home for emergencies?
Yes, if prescribed and stored according to DEA rules. Schedule II opioids (like oxycodone) must be kept in a substantially built, locked cabinet, separate from other medications. Keys or access codes must be limited to the patient and one other authorized person. Never leave them on a counter, even for a minute. Theft or loss must be reported to the DEA and local police immediately.
How often should I check my emergency meds?
Check expiration dates every 3 months. Look for discoloration, leaks, or strange smells. Replace epinephrine or insulin if the liquid looks cloudy or has particles. Even if it hasn’t expired, heat or age can weaken it. Replace any med that’s been exposed to extreme temperatures.
What if I’m not sure how to store a specific medication?
Call the pharmacy that filled the prescription. They’re required to give you storage instructions. You can also contact the manufacturer directly-most have customer service lines. The FDA’s 2023 guidance says 57% of patients are unsure about storage, so you’re not alone. Don’t guess. Ask.

Comments (10)