By 2025, detecting cognitive decline isn’t about waiting for someone to forget their grandchild’s name. It’s about catching tiny, invisible changes in the brain before they turn into memory loss or confusion. That shift is happening fast - and it’s changing everything for older adults, families, and doctors.
Why Screening Matters More Than Ever
Most people think cognitive decline only becomes a problem when memory starts slipping badly. But the truth? Brain changes begin years, sometimes decades, before symptoms show. By the time someone struggles to pay bills or gets lost walking to the corner store, the disease has already advanced.
Now, with new drugs like lecanemab that slow Alzheimer’s progression, catching early signs isn’t just helpful - it’s critical. These treatments work best when started in the earliest stage: mild cognitive impairment (MCI). That’s why doctors are no longer waiting for red flags. They’re looking for whispers - subtle changes in thinking that paper tests used to miss.
Old Tests Are Out. New Tools Are In.
For years, the Montreal Cognitive Assessment (MoCA) and Mini-Cog were the go-to tools. They asked people to draw a clock, remember three words, or name animals. Simple. Quick. But they’re outdated.
Here’s why: a 2023 meta-analysis found MoCA only catches about 80% of early MCI cases. That means one in five people with early brain changes slip through. And those tests can’t tell the difference between a tired 75-year-old and someone with Alzheimer’s pathology. They measure outcomes, not how the brain gets there.
Today, the real game-changers are digital tools that track how you do things - not just whether you get the right answer.
- Linus Health’s DAC takes just 7 minutes. It combines a digital clock-drawing test with a trail-making task that measures every millisecond of your pen movement - speed, pressure, hesitations. Machine learning spots patterns no human can see.
- Cleveland Clinic’s C3B has a 92% completion rate in clinics. It’s built into the Medicare annual wellness visit, so doctors track your scores year after year. A drop of even 2 points over 12 months can signal trouble.
- VR-E uses virtual reality and eye-tracking. You watch a 3D street scene and answer questions. The system tracks where you look, how long you pause, and if you miss details. It spots spatial confusion before you even realize you’re getting lost in familiar places.
These tools don’t just detect MCI - they distinguish between normal aging and early disease with 90%+ accuracy. One study showed VR-E’s AUC of 0.9415. That’s better than most blood tests for cancer.
What’s Being Measured? The Hidden Details
Traditional tests ask: “What’s the date?”
New tools ask: “How long did it take you to draw that clock? Did your pen shake? Did you erase twice? Did you start from the outside and work inward, or jump around?”
That’s the difference. Digital tools capture process, not just result.
For example, the digital Trail Making Test (dTMT-B) measures:
- Total time to complete (milliseconds)
- Stroke velocity (how fast your pen moves)
- Drawing efficiency (how close your path is to the ideal route)
- Pauses between numbers
A healthy person draws smoothly, with steady speed. Someone with early cognitive decline might pause repeatedly, backtrack, or rush the last few numbers. These aren’t “mistakes” - they’re biomarkers. And they’re 87% accurate at telling neurocognitive decline apart from arthritis or slow reflexes.
Real People, Real Experiences
Patients aren’t resisting these tools - they’re embracing them.
In Cleveland Clinic’s clinics, 68% of patients said they felt less anxious than with paper tests. One 78-year-old woman used Linus Health’s app in her doctor’s waiting room - no help needed. “I thought it was a game,” she said. “Then the doctor said, ‘Your results are normal, but let’s check again next year.’”
On Reddit, caregivers report similar stories. “My dad thought the tablet was for kids,” wrote one user. “But he completed it in 5 minutes and didn’t even realize it was a test.”
But it’s not perfect. About 17% of users struggle with button clicks or small fonts. One man failed a test because he couldn’t tap the screen - not because he forgot his daughter’s name, but because the interface wasn’t designed for shaky fingers or poor eyesight.
That’s why the best tools now have voice guidance, larger buttons, and adjustable contrast. And doctors are learning to help. “We don’t just hand someone a tablet,” says a nurse in Minneapolis. “We sit with them. We say, ‘This is just like checking your blood pressure. It’s part of staying healthy.’”
Doctors Are Adopting - But Not Everywhere
Primary care doctors used to say, “I don’t have time for cognitive tests.” Now, many are doing them during Medicare annual visits. Why? Because CMS now pays up to $45 per test. And because tools like C3B take less than 10 minutes.
Training is simple: 15 minutes for physicians, 20 minutes for medical assistants. Cleveland Clinic rolled it out to 200 clinics in 6 months. Adoption hit 91%.
The biggest hurdle? Getting the results into electronic health records. About 67% of health systems still struggle with this. If the test result doesn’t pop up in the doctor’s chart, it’s useless. The solution? Custom integrations. Some clinics now auto-flag scores that drop below baseline - so doctors see it before the patient even walks out.
The Future: Blood Tests and AI Combined
The next leap isn’t just digital screens - it’s blood.
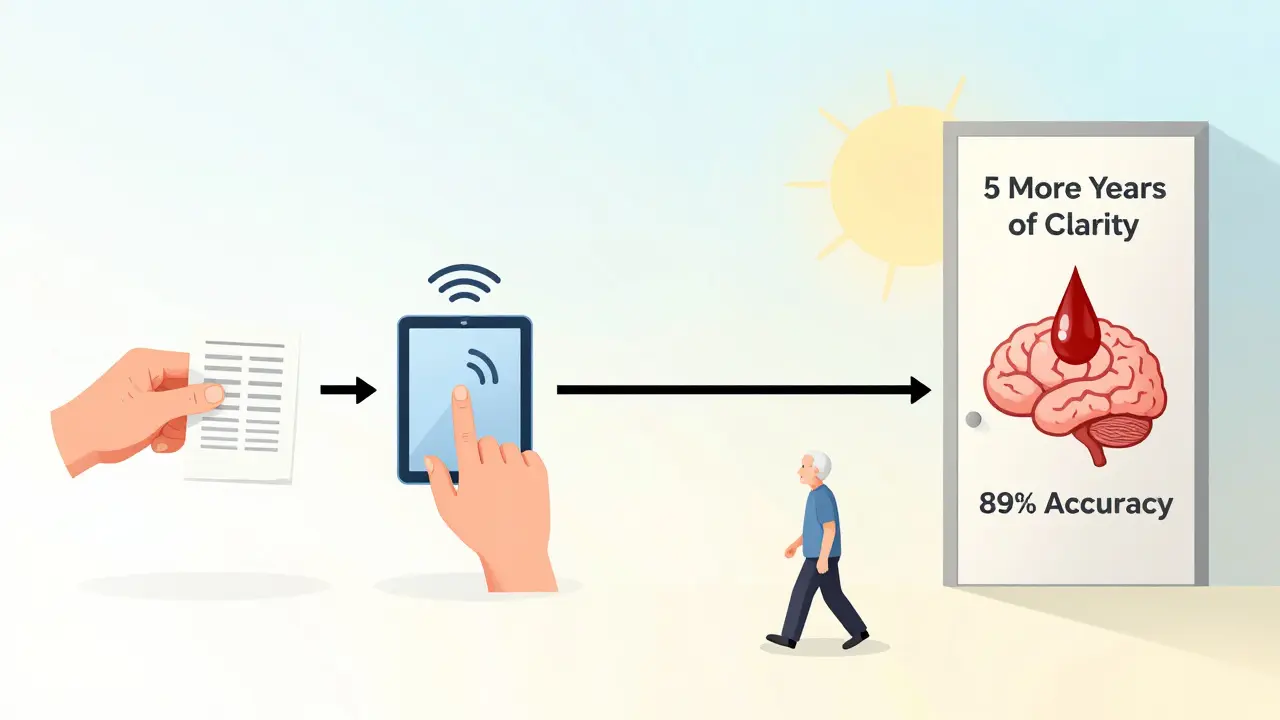
For years, diagnosing Alzheimer’s meant expensive PET scans or spinal taps. Now, blood tests can detect amyloid and tau proteins - the same markers found in the brain. In 2025, several are approved for clinical use.
Linus Health already combines its digital tests with APOE gene status and blood biomarkers. Their model predicts brain amyloid levels with 89% accuracy - nearly matching PET scans.
That’s huge. Imagine: a simple blood draw, a 7-minute tablet test, and your doctor knows if you’re on the path to Alzheimer’s - five years before memory loss starts.
But caution remains. Dr. Ronald Petersen of Mayo Clinic warns: “We can’t assume every digital change means Alzheimer’s pathology.” Some people show digital signs of decline but never develop dementia. Others have plaques in their brain but no symptoms. That’s why tools must be validated against actual brain biomarkers - not just other tests.
What You Can Do Today
If you’re over 60 - or care for someone who is - here’s what matters now:
- Ask your doctor if they use a digital cognitive screen during your annual wellness visit. If not, ask why.
- Don’t wait for memory lapses. If you’ve noticed small changes - forgetting names, losing track in conversations, struggling with bills - speak up. These are red flags.
- Know that digital tools aren’t perfect, but they’re better than what came before. If you’re uncomfortable with a tablet, ask for a paper version - but insist on follow-up.
- Track your results. A single test doesn’t diagnose. Trends over time do. Keep copies of your scores.
And if your doctor says, “It’s just aging”? Push back. Aging isn’t forgetting your password. It’s not needing to write down every appointment. Those are signs - and now, we have the tools to see them early.
What’s Next?
By 2030, digital cognitive screening will be as routine as cholesterol checks. Medicare will cover it. Insurance will follow. And the goal won’t be just diagnosis - it’ll be prevention.
Early detection means early action. And early action means more years of independence, connection, and clarity.
What’s the difference between normal aging and MCI?
Normal aging means taking longer to recall a name or forgetting where you put your glasses. MCI is when these lapses start affecting daily life - like forgetting appointments regularly, struggling to follow conversations, or having trouble managing finances. The key difference? MCI shows up on sensitive cognitive tests, even if you’re still independent. It’s a warning sign - not a diagnosis of dementia.
Are digital cognitive tests reliable?
Yes - if they’re validated. Tools like Linus Health’s DAC, Cleveland Clinic’s C3B, and VR-E have been tested in peer-reviewed studies against gold-standard neuropsychological exams and brain biomarkers. They’re more accurate than MoCA or Mini-Cog. But not all apps are created equal. Stick to tools used in clinics or recommended by your doctor. Avoid consumer apps that claim to “prevent dementia” - most aren’t scientifically backed.
Can I do a cognitive test at home?
Some tools, like RoCA or Linus Health’s app, are designed for home use. But they’re not meant to replace a clinical evaluation. Home tests are best for tracking changes over time - not diagnosing. If you notice a decline in your scores, see your doctor. A single low score could be from stress, sleep loss, or medication - not dementia.
Does Medicare cover cognitive screening?
Yes. Medicare covers annual wellness visits that include cognitive assessment. As of 2025, CMS reimburses up to $45 per validated digital cognitive test when performed during these visits. The test must be administered by a qualified provider - not self-administered at home - to qualify for payment.
What if I’m not tech-savvy?
You don’t need to be. Most digital tools are designed for older adults - big buttons, voice prompts, simple navigation. Many clinics have staff help you through it. If you’re uncomfortable, ask for a paper version. But don’t skip the test. The goal is early detection, not perfect tech skills. Your doctor’s team can help you use the tool - it’s their job.
Are these tests only for Alzheimer’s?
No. While they’re often used for Alzheimer’s, these tools can detect early signs of other conditions - vascular dementia, Lewy body dementia, frontotemporal dementia, and even depression-related cognitive fog. The pattern of errors helps doctors tell them apart. That’s why detailed digital metrics matter - they give clues to the underlying cause.
Final Thought: It’s Not About Fear - It’s About Control
Cognitive decline doesn’t have to be a surprise. With today’s tools, you can know - and act - before it steals your independence. This isn’t about predicting the future. It’s about protecting the present. The next time you’re at your annual checkup, ask: “Did you check my brain today?” You’ve got nothing to lose - and years to gain.


Comments (11)
It's fascinating how the metrics have evolved from 'can you draw a clock' to analyzing millisecond-level pen pressure. This isn't just progress-it's a paradigm shift in neurology. The fact that we can now distinguish between vascular cognitive impairment and early Alzheimer's through movement patterns is nothing short of revolutionary. I've seen too many patients dismissed as 'just getting older' when their dTMT-B scores showed clear deviations. We need to standardize these tools universally, not just in academic clinics.
I'm so tired of doctors brushing off memory lapses as 'normal aging.' My mom took the VR-E test last month-she thought it was a puzzle game. When the doctor said her spatial navigation score had dropped 18% in a year, she cried. Not from fear-from relief. Finally, someone saw what was happening. These tools give us back agency. If your doctor doesn't offer this, find one who does. Your future self will thank you.
It’s interesting how we’ve moved from measuring outcomes to measuring process. The clock-drawing test asked: 'Can you do it?' The new tools ask: 'How do you do it?' That’s the difference between judging a result and understanding a journey. It reminds me of how we used to diagnose depression by counting symptoms-now we track sleep patterns, micro-expressions, even keystroke variability. The brain isn’t a black box anymore. We’re learning to read its language.
If you’re over 60 and haven’t asked your doctor about cognitive screening, please do it today. Not because you’re scared-but because you deserve to know. These aren’t scary tests; they’re like checking your cholesterol. And if you’re helping someone older, don’t assume they can’t use a tablet. My 82-year-old uncle did the Linus test in under 6 minutes. He said, 'That was easier than my banking app.' We just need to stop treating older adults like they’re broken.
Let’s be honest: most of these 'breakthrough' digital tools are just rebranded psychometric assessments with machine learning lipstick. The AUC of 0.9415 sounds impressive until you realize it’s still a proxy. We’re not measuring amyloid burden-we’re measuring behavioral artifacts. And let’s not forget: correlation is not causation. Many elderly patients show 'decline' on these screens due to depression, polypharmacy, or sleep apnea. The real danger isn’t missing MCI-it’s overdiagnosing it and medicating people who don’t need it.
Wait-you’re telling me a 78-year-old woman thought this was a game? That’s not a win, that’s a failure of design. If you need to trick elderly people into taking a medical test by making it look like Candy Crush, the system is broken. And why is CMS paying $45 per test? Because it’s a revenue stream, not a health intervention. These tools are being pushed because they’re billable, not because they’re clinically superior. I’ve seen patients traumatized by false positives. This isn’t progress-it’s monetized anxiety.
My grandma did the C3B test last week. She was nervous, so the nurse sat with her and said, 'Just pretend you're playing a quiet game.' She finished it in 4 minutes. The next day, she said, 'I didn't know they could tell how fast I think.' That hit me hard. We spend so much time worrying about the diagnosis, but the real gift is giving people awareness. Even if nothing changes, knowing you're still sharp? That’s dignity.
One thing everyone’s missing: these tools are only as good as the baseline. A single test means nothing. What matters is trend data. I’ve seen patients whose scores dropped 2 points over 18 months-no symptoms, no complaints. But that dip? That’s the window for intervention. The real value isn’t in the test-it’s in longitudinal tracking. If your doctor isn’t saving your results year over year, you’re not getting the full benefit. Keep copies. Ask for graphs. Make it part of your health record.
As someone from India, I’m glad to see these tools being adopted. But we need to consider cultural and linguistic bias. The clock-drawing test assumes familiarity with analog clocks. Many older adults in rural areas have never used one. The VR-E test assumes spatial navigation in Western-style streets. We need localized versions-voice-guided, culturally adapted. Technology shouldn’t exclude the very people it aims to help.
It is, indeed, a matter of profound significance that the medical community has, in recent years, begun to embrace the notion that cognitive health is not merely an ancillary concern, but a cornerstone of geriatric care. The transition from antiquated, subjective, and often culturally biased paper-based assessments to digitally nuanced, algorithmically validated, and statistically robust instruments represents nothing short of a renaissance in neuropsychological evaluation. The fact that such tools now possess the capacity to discern subtle, millisecond-level variations in motor-executive function-thereby differentiating between normative aging and neurodegenerative pathology with an AUC exceeding 0.94-is, frankly, a triumph of biomedical engineering and clinical foresight. One can only hope that reimbursement models, electronic health record integration, and provider education will evolve at a commensurate pace to ensure equitable access across socioeconomic strata.
my dad did the test last week and he said it was kinda fun, like a brain workout. he didn’t even know it was a test! the doc said his score was good but to come back in 6 months. i think this is the future. no more waiting till someone forgets your name. just check it like a blood test. also, the buttons were big, no problem with his hands. thanks for sharing this!