Every pill you swallow, every injection you get, every inhaler you use - it’s not magic. It’s chemistry. Medicines work because they’re designed to interact with your body at a molecular level. But knowing how medicines work isn’t just for doctors. It’s the key to using them safely - and avoiding dangerous mistakes.
What Happens When You Take a Pill?
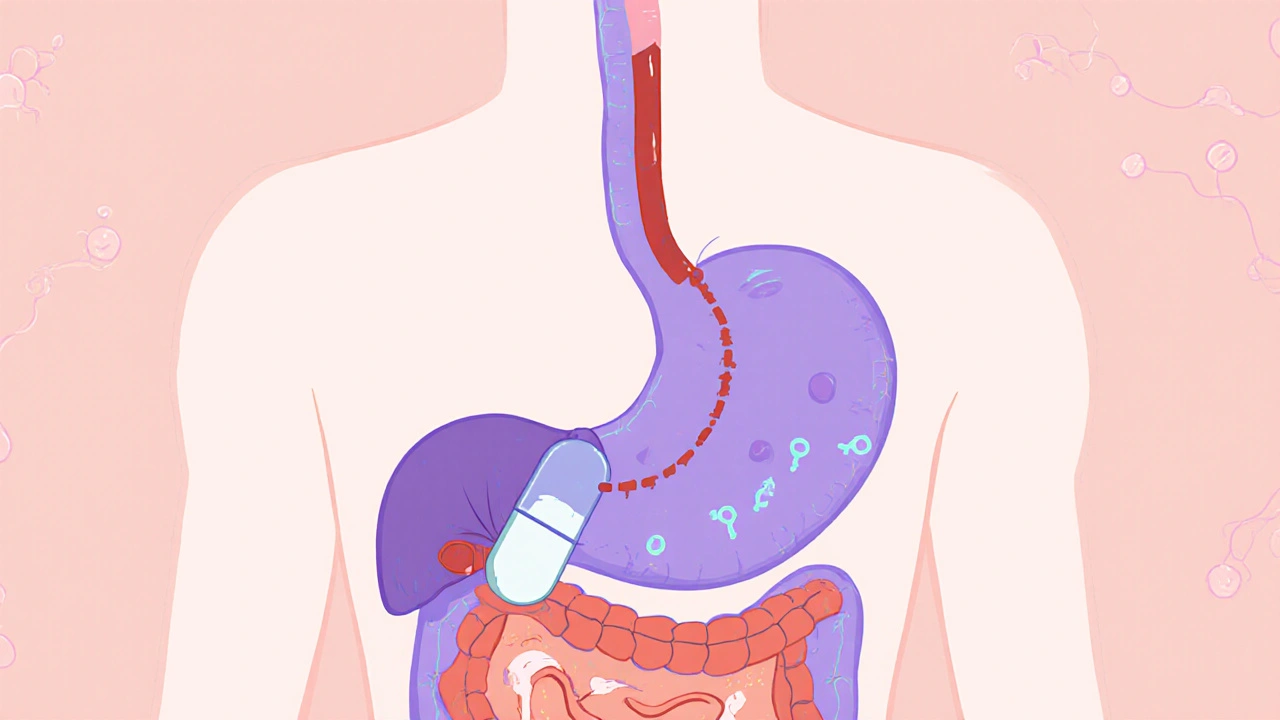
When you swallow a tablet, it doesn’t just float around waiting to do something. It travels. First, it breaks down in your stomach and intestines. Then, it gets absorbed into your bloodstream. But here’s the catch: not all of it makes it to work. Some drugs get broken down by your liver before they even reach your target. This is called the first-pass effect. For example, propranolol loses up to 90% of its strength before it ever reaches your heart. That’s why some pills need higher doses than others.Once in the blood, most drugs bind to proteins - often 95% or more. Only the small unbound portion is active. That’s why two people taking the same dose might feel very different effects. One might have more free drug circulating because their protein levels are lower. Or because they’re taking another drug that pushes the first one off the protein.
Then comes the real target: receptors. Think of them like tiny locks on the surface of your cells. Medicines are the keys. Some keys, like serotonin reuptake inhibitors (SSRIs), fit perfectly into the lock and block the door from closing. That’s how fluoxetine (Prozac) keeps more serotonin in your brain - helping with depression. Others, like aspirin, don’t just open a door - they break the lock permanently. Aspirin shuts down the COX-1 enzyme, stopping the production of pain signals and inflammation. That’s why one dose can last hours.
Why Some Drugs Are Safe - and Others Aren’t
Not all drugs are created equal in terms of safety. The difference often comes down to how precisely they target their job.Take statins. They block HMG-CoA reductase, an enzyme your liver uses to make cholesterol. Because scientists know exactly how this works, they can monitor your cholesterol levels and adjust your dose. If your cholesterol drops too low, they reduce the dose. If it’s still high, they increase it. That’s precision medicine.
Now compare that to lithium, used for bipolar disorder. No one fully understands how it works. It affects dozens of pathways in the brain. That’s why the safe range is razor-thin: 0.6 to 1.2 mmol/L in your blood. Go just a little above that, and you risk tremors, confusion, or even kidney damage. Go below, and it does nothing. That’s why people on lithium need regular blood tests - every few weeks, sometimes monthly.
Even worse are drugs with unclear mechanisms. Dimebon, once tested for Alzheimer’s, showed early promise but failed in large trials. Why? Because no one knew how it worked. If you don’t know how a drug acts, you can’t predict side effects, interactions, or who will benefit. That’s why the FDA now requires detailed mechanism of action (MOA) data for nearly all new drugs - up from 62% in 2015 to 87% today.
When Medications Become Dangerous
Medications are safe - until they’re not. And often, the danger comes from things you don’t realize are connected.Warfarin, a blood thinner, blocks vitamin K. That’s good - it stops clots. But if you suddenly eat a big salad with spinach, kale, or broccoli - all packed with vitamin K - the drug loses power. Your blood starts clotting again. On the flip side, if you stop eating greens for weeks, warfarin becomes too strong. You could bleed internally. That’s why patients on warfarin are told to keep their diet steady. And why they’re taught to recognize signs of bleeding: unusual bruising, dark stools, headaches that won’t quit.
MAO inhibitors for depression are another example. These drugs stop your body from breaking down tyramine, a chemical found in aged cheeses, cured meats, and tap beer. If you eat these while on MAOIs, tyramine builds up and causes a sudden, dangerous spike in blood pressure. One study found that 32% of adverse drug reports involved patients who didn’t know this connection. They thought, “It’s just cheese,” and ended up in the ER.
Even over-the-counter drugs can be risky. Mixing NSAIDs like ibuprofen with blood thinners increases bleeding risk. Taking acetaminophen with alcohol can damage your liver. These aren’t random side effects - they’re predictable results of how the drugs interact with your body’s chemistry.
Why Understanding Your Medicine Changes Everything
Knowing how your medicine works isn’t just academic. It saves lives.A 2023 survey by the American Cancer Society found that 78% of patients on trastuzumab (Herceptin) for HER2-positive breast cancer felt more confident about treatment when they understood it targeted a specific protein on cancer cells. They knew to watch for heart problems - a known side effect - because the drug affects heart muscle receptors too. Those who didn’t understand the mechanism were less likely to spot early warning signs.
On PatientsLikeMe, 68% of users said they worried about side effects. But 42% said that if they understood how their drug worked, they could tell the difference between normal reactions and real danger. One man on statins told his pharmacist he’d been ignoring muscle pain for months. When he learned statins block cholesterol production - but also affect muscle energy pathways - he realized the pain wasn’t just “getting older.” He got tested. His CPK levels were high. He caught early rhabdomyolysis. He avoided kidney failure.
Community pharmacists report that when they use simple analogies - like “SSRIs are like putting a cork in the serotonin recycling tube” - patients understand why suddenly stopping the drug causes dizziness, nausea, or brain zaps. They don’t think they’re going crazy. They know it’s a chemical withdrawal.

What You Can Do Right Now
You don’t need a science degree to use medicine safely. But you do need to ask the right questions.- What is this drug supposed to do in my body? Don’t settle for “it treats high blood pressure.” Ask: “Does it relax my arteries? Block a hormone? Reduce fluid?”
- What foods, drinks, or other meds should I avoid? If you’re on warfarin, ask about vitamin K. If you’re on an antibiotic, ask about dairy or alcohol. If you’re on antidepressants, ask about painkillers or supplements like St. John’s Wort.
- What side effects mean I need to call my doctor? Is it normal to feel tired? Or is sudden swelling a red flag? Know the difference.
- Is there a blood test to monitor this? For lithium, warfarin, statins, and some seizure meds - yes. Ask if you should get checked regularly.
Don’t be shy. Pharmacists are trained to explain this stuff. Most spend nearly 9 minutes per patient just on safety explanations. They use diagrams. They draw pictures. They want you to understand.
The Future of Safe Medication Use
Science is getting smarter. The NIH’s All of Us program is collecting genetic data from a million people to see how your DNA affects how you respond to drugs. Already, 28% of bad reactions are linked to gene variations that change how your body processes medicine.By 2028, we may see “digital twins” - computer models of your body that simulate how a drug will affect you before you even take it. That could cut adverse events by half.
But until then, the safest way to use medicine is simple: know how it works. Understand the mechanism. Ask questions. Don’t assume. Don’t guess. Your body isn’t a black box. It’s a complex, predictable system. And when you understand the rules, you can play the game safely.

Comments (8)
Man, I wish my doctor explained meds like this. I took statins for years and never knew why my muscles hurt until I read this. Now I get it - it’s not just aging, it’s the energy pathways getting blocked. Should’ve asked sooner.
Wow. Just... wow. 😮 I didn’t realize SSRIs were like putting a cork in a recycling tube… that’s so simple, yet so accurate. I’ve had brain zaps before-thought I was losing my mind. Now I know it’s just chemistry. Thank you.
This is exactly the kind of clear, science-backed explanation we need more of. The first-pass effect alone is something every patient should understand-especially when they wonder why their dose seems so high. Precision matters. And so does knowing that 95% of your drug is just hitching a ride on proteins until it’s time to act. Brilliant breakdown.
lol so now we’re all supposed to be biochemists just to take a pill? Next they’ll make us memorize enzyme names before we can buy ibuprofen. 🤡
Let’s not ignore the elephant in the room: the pharmaceutical industry’s obsession with mechanism-of-action data is less about safety and more about patent extension. If they can’t patent a mechanism, they can’t monopolize the market. The FDA’s 87% requirement? A corporate maneuver disguised as public health.
LOL all this ‘understanding your medicine’ nonsense. 😂 In India, we just take what the doctor gives and don’t ask why. Most people don’t even know what ‘receptors’ are. And guess what? They live just fine. This over-intellectualizing is a Western luxury.
THIS. IS. A. MASTERPIECE. 🎭 The way aspirin doesn’t just open a door-it SMASHES the lock? The serotonin cork? The warfarin-and-salad drama that could KILL YOU? I’m not just reading this-I’m living it. My aunt nearly bled out because she ate kale and didn’t know. This isn’t science. This is a thriller. Someone turn this into a Netflix doc. I’ll watch it. I’ll cry. I’ll share it with my entire family.
The assertion that understanding mechanism improves adherence and safety is supported by empirical evidence, as cited. However, one must acknowledge that accessibility to such knowledge remains inequitable across socioeconomic strata. The burden of comprehension should not rest solely upon the patient, but be actively facilitated by the healthcare system through standardized educational protocols. A commendable article, though lacking in structural policy critique.