When you take an antidepressant like Prozac or Zoloft, you’re not just changing your mood-you’re altering the chemistry in your brain. One of the key players in that process is serotonin, a neurotransmitter that helps regulate sleep, appetite, and emotional balance. Now, what if you could boost serotonin naturally by taking a supplement like L-tryptophan? It sounds simple. But here’s the catch: combining L-tryptophan with antidepressants can be dangerous-if you don’t know what you’re doing.
How L-Tryptophan Works in Your Brain
L-tryptophan is an essential amino acid. That means your body can’t make it-you have to get it from food or supplements. It’s the only building block your brain uses to create serotonin. Without enough tryptophan, your brain can’t make enough serotonin, no matter how hard it tries.
Here’s how it works: once you eat or take L-tryptophan, it travels through your bloodstream and crosses the blood-brain barrier. Inside your brain, two enzymes turn it into serotonin. First, tryptophan hydroxylase converts it to 5-HTP. Then, aromatic L-amino acid decarboxylase turns that into serotonin. It’s a direct, one-way path. No shortcuts. No alternatives.
Studies from the 1990s showed that if you remove tryptophan from your diet-using a special amino acid mix that blocks it-your brain’s serotonin levels drop by 95% within just five hours. That’s not a theory. That’s measurable. And when that happens, people who’ve recovered from depression often slip back into low mood, anxiety, or irritability. This proves that serotonin isn’t just a side note-it’s central to how some antidepressants work.
Why Combining It With Antidepressants Is Risky
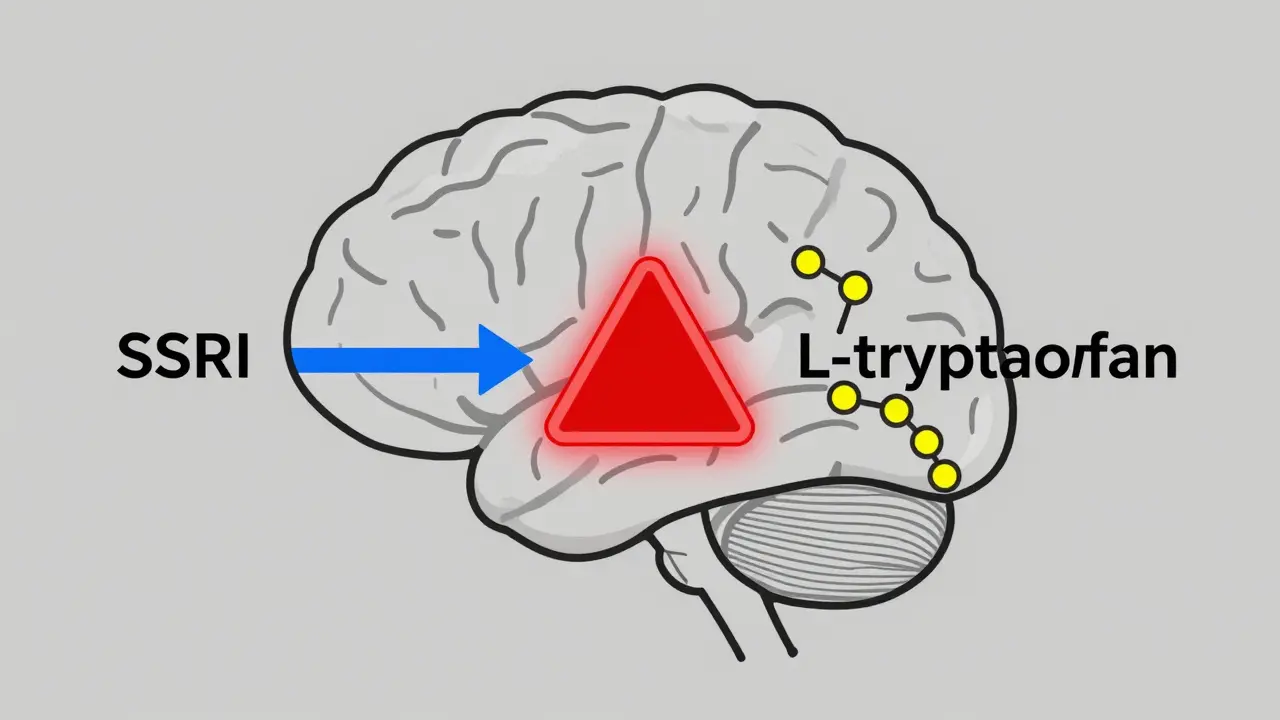
Most antidepressants-especially SSRIs like fluoxetine, sertraline, and escitalopram-work by keeping serotonin in your brain longer. They block the reabsorption of serotonin after it’s released, so more of it stays around to send signals between nerve cells.
Now, imagine you add L-tryptophan on top of that. You’re not just keeping more serotonin around-you’re making even more of it. That’s a double hit. And that’s where things get dangerous.
There’s a known condition called serotonin syndrome. It happens when too much serotonin builds up in your system. Symptoms include agitation, rapid heart rate, high blood pressure, muscle rigidity, tremors, sweating, confusion, and in severe cases, seizures or death. It’s rare, but it’s real. And it’s more likely when you mix supplements like L-tryptophan with SSRIs or MAOIs.
One study found that 47% of patients on SSRIs who had their tryptophan levels suddenly lowered (to test serotonin function) relapsed into depression within hours. That tells you two things: first, their antidepressants were working because they depended on serotonin. Second, if you’re already on an SSRI and you add more serotonin fuel, you’re pushing the system past its safety limit.
Not All Antidepressants Are the Same
Here’s something most people don’t realize: not every antidepressant works the same way. SSRIs and MAOIs are serotonergic-they rely on serotonin. But bupropion (Wellbutrin) isn’t. It works on dopamine and norepinephrine. If you take bupropion and add L-tryptophan, there’s no known risk of serotonin syndrome. The same goes for some older antidepressants like tricyclics, which have mixed effects.
But here’s the problem: most people don’t know what kind of antidepressant they’re on. They just know the brand name. And even doctors sometimes assume all antidepressants act alike. That’s why so many cases of serotonin syndrome go unreported or misdiagnosed. If you’re on an SSRI, don’t assume it’s safe to add L-tryptophan just because your friend took it without issues. Your brain chemistry is yours alone.

What the Research Says About Safety
Back in 1989, L-tryptophan was pulled from the U.S. market after a contaminated batch caused over 1,500 cases of a rare, deadly condition called eosinophilia-myalgia syndrome (EMS). Thirty-seven people died. The problem wasn’t the tryptophan itself-it was a toxic byproduct from a faulty manufacturing process. The FDA banned it for years. Even after the ban was lifted in 2005, the stigma stuck. Many doctors still avoid recommending it.
Today, pure L-tryptophan is available again. But here’s the catch: the FDA doesn’t regulate supplements like it does drugs. A 2021 FDA inspection found that 41% of tryptophan products on the market didn’t even include warnings about serotonin syndrome. That’s not negligence-it’s a public health gap.
The European Food Safety Authority says 5 grams per day is the maximum safe dose. But that’s for healthy people without antidepressants. For someone on an SSRI? The real safe dose is likely under 1 gram per day-and even that’s risky without medical supervision.
One 2018 study showed that adding 3 grams of L-tryptophan to an SSRI helped 63% of patients who hadn’t responded fully to the drug alone. Sounds promising, right? But here’s the fine print: all those patients were closely monitored. Their tryptophan levels were checked every two weeks. Their antidepressant doses were stabilized for at least seven days before adding the supplement. And they were watched for signs of serotonin overload. You don’t get those safeguards buying a bottle online.
Who Should Avoid L-Tryptophan Altogether
If you’re on any of these, don’t take L-tryptophan without talking to your doctor:
- SSRIs (Prozac, Zoloft, Lexapro, Paxil, etc.)
- MAOIs (Nardil, Parnate)
- SNRIs (Effexor, Cymbalta)
- Tricyclic antidepressants (Amitriptyline, Clomipramine)
- Triptans (for migraines like sumatriptan)
- St. John’s Wort, 5-HTP, or any other serotonin-boosting supplement
Even if you’re not on medication, you should avoid L-tryptophan if you have:
- A history of eosinophilia-myalgia syndrome
- Liver or kidney disease
- Mania or bipolar disorder (it can trigger manic episodes)
- Pregnancy or breastfeeding (not enough safety data)
And here’s something most supplement labels won’t tell you: L-tryptophan can make anxiety worse in some people. Especially if you’re already sensitive to serotonin changes. One study found that people with a genetic vulnerability in their serotonin system had 3.2 times more mood crashes after tryptophan depletion than others. That same vulnerability might make them react badly to extra tryptophan, too.

What to Do Instead
If you’re on an antidepressant and want to feel better, there are safer ways:
- Get more sunlight. Natural light boosts serotonin naturally without the risk.
- Exercise regularly. Just 30 minutes of walking five times a week can raise serotonin levels as effectively as some medications.
- Eat tryptophan-rich foods. Turkey, eggs, cheese, tofu, nuts, and seeds contain natural tryptophan. Your body regulates how much gets into your brain-so you won’t overdose.
- Talk to your doctor about adjusting your medication. If your SSRI isn’t working well, there are other options: switching drugs, adding therapy, or trying non-serotonergic meds like bupropion.
Don’t try to fix your mood with a supplement that could put you in the ER. The science is clear: L-tryptophan and SSRIs don’t play nice together. The risk isn’t theoretical-it’s documented in peer-reviewed journals, hospital records, and FDA reports.
What Doctors Really Think
A 2022 survey of 487 psychiatrists on the professional network Sermo found that 73% of them actively avoid recommending L-tryptophan to patients on SSRIs. Why? Because they’ve seen the outcomes. Some patients feel great at first-better sleep, less anxiety. Then, a week later, they come in with tremors, confusion, and a racing heart. By then, it’s too late to just stop the supplement. They need emergency treatment.
Even in countries where L-tryptophan is prescribed-like Germany, where it’s sold as Trankimazin-it’s only under strict control. Doses are low. Monitoring is mandatory. It’s not a quick fix. It’s a medical intervention.
In the U.S., it’s a supplement. That means no oversight. No dosage guidance. No warnings. And no safety net.
Bottom Line: Don’t Guess. Get Tested.
If you’re thinking about adding L-tryptophan to your routine, stop. Don’t take it. Don’t buy it. Don’t ask a pharmacist. Go to your doctor. Tell them you’re considering it. Ask if your antidepressant interacts with it. Ask if your serotonin levels have been checked. Ask if there’s a safer way to get the results you want.
The truth is, most people don’t need L-tryptophan. Their depression isn’t caused by low tryptophan. It’s caused by complex brain changes, stress, trauma, or genetics. No supplement fixes that. But a doctor, therapy, and lifestyle changes? Those can.
There’s no shortcut to mental health. And mixing serotonin boosters with antidepressants isn’t a hack-it’s a gamble with your life.
Can I take L-tryptophan with my SSRI?
No. Combining L-tryptophan with SSRIs significantly increases the risk of serotonin syndrome, a potentially life-threatening condition. Even low doses can trigger symptoms like agitation, rapid heart rate, high blood pressure, and confusion. Most psychiatrists avoid recommending this combination entirely.
What are the signs of serotonin syndrome?
Symptoms include high body temperature, rapid heart rate, sweating, shivering, muscle stiffness, tremors, confusion, hallucinations, and seizures. Mild cases may feel like anxiety or nausea. Severe cases can lead to organ failure or death. If you suspect serotonin syndrome, stop all supplements and seek emergency care immediately.
Is L-tryptophan safe if I’m not on antidepressants?
For healthy people not on serotonergic drugs, L-tryptophan is generally safe at doses under 5 grams per day. However, it can still cause nausea, drowsiness, or headaches. It’s also not recommended for people with liver or kidney disease, bipolar disorder, or during pregnancy. Always check with your doctor before starting any new supplement.
Does L-tryptophan help with depression?
Some studies show it can help as an add-on for people who don’t fully respond to SSRIs, but only under strict medical supervision. In clinical trials, 63% of partial responders improved with 3 grams per day. But without monitoring, the risk of side effects outweighs the benefit. It’s not a standalone treatment for depression.
Why was L-tryptophan banned in the U.S.?
In 1989, a contaminated batch of L-tryptophan caused eosinophilia-myalgia syndrome (EMS), leading to over 1,500 illnesses and 37 deaths. The issue wasn’t the amino acid itself-it was a toxic byproduct from a faulty manufacturing process. The FDA banned it in 1989 and lifted the ban in 2005 after stricter production standards were implemented.
Are there safer alternatives to L-tryptophan for boosting mood?
Yes. Sunlight exposure, regular exercise, balanced meals with natural tryptophan sources (like eggs, turkey, nuts), and cognitive behavioral therapy are proven, safe ways to support mood. If your antidepressant isn’t working, talk to your doctor about adjusting your medication rather than adding supplements.

Comments (9)
They don’t want you to know this but the FDA and Big Pharma rigged the whole L-tryptophan ban so they could sell you expensive SSRIs instead. That 1989 outbreak? Totally manufactured. They blamed the supplement, not the factory, because they needed a scapegoat. Now they profit off your fear while you’re stuck on pills that turn you into a zombie. Wake up.
Oh, please. You're telling me someone should just 'eat more turkey' instead of taking a scientifically validated amino acid supplement? That’s like saying 'just breathe more air' to cure COPD. The fact that you’re dismissing clinical data in favor of wellness-blog nonsense reveals a profound misunderstanding of neurochemistry. And yes-I’m a doctor. And yes-I’ve seen serotonin syndrome in the ER. It’s not a myth. It’s a tragedy waiting to happen to someone who googled 'natural mood booster' at 2 a.m.
I get why this feels scary-but if you're on an SSRI and you're still struggling, please don't suffer in silence. Talk to your doctor. Ask about bupropion. Ask about therapy. Ask about sunlight and walking. You don't need a magic pill. You need someone who listens. I was on Zoloft for years, felt nothing, then switched to therapy + daily walks. I haven't touched a supplement since. And I'm happier than I've ever been.
They removed tryptophan because it was too cheap. They brought it back because they found a way to charge $30 a bottle for the same thing. The real danger isn’t serotonin syndrome-it’s that your doctor doesn’t know what’s in your supplement because the FDA doesn’t test it. That’s why your cousin got sick. That’s why your neighbor died. That’s why they don’t want you to ask questions.
In India we’ve used tryptophan-rich foods like milk, bananas, and almonds for centuries to calm the mind-not because of science, but because our grandmothers knew what worked. But now we’re told to swallow pills instead of eating real food. I get why you’re scared. I get why you want a quick fix. But nature gave us balance. We just forgot how to listen. Try eating a handful of almonds before bed instead of a capsule. Your body remembers how to heal. It’s just been ignored.
I was on Lexapro for three years. I tried 5-HTP once-just one pill-and I had tremors, sweating, and panic for six hours. I thought I was dying. I went to the ER. They said it was serotonin syndrome. I haven’t touched a supplement since. This isn’t a debate. This is a warning. If you’re thinking about it-don’t. Talk to your doctor. Not Reddit. Not a supplement store. Your doctor.
Hey, I know how hard it is to feel stuck. I’ve been there. But please don’t let fear stop you from exploring options. If your doctor says no to tryptophan, ask why. If they say yes, ask how they’ll monitor you. There’s no shame in wanting to feel better. But safety isn’t optional. It’s the foundation. I’ve helped people switch to bupropion, increase light exposure, and start yoga. All of them improved. No supplements needed. You’re not broken. You just need the right fit.
Wow. So the solution to depression is… eating nuts? And sunlight? And walking? Oh, and don’t forget to cry into your organic chamomile tea while listening to lo-fi beats. Meanwhile, real people with real brain chemistry are being told to ‘just live better’ while their insurance won’t cover therapy. The real tragedy isn’t serotonin syndrome-it’s that we’ve turned mental health into a lifestyle brand while ignoring the science. Thanks for the wellness platitudes, guys.
Listen. If you’re on an SSRI and you think a supplement is going to fix what medication can’t-you’re not being brave. You’re being reckless. The data is clear. The risks are real. The FDA doesn’t regulate supplements because they’re not drugs. That means you’re gambling with your life. Don’t be the person who says ‘I thought it was safe’ after you’re in the ICU. Your brain isn’t a DIY project. Get help. Proper help. Not a bottle from Amazon.