Nighttime Hypoxia: What It Is, Why It Matters, and How to Spot It
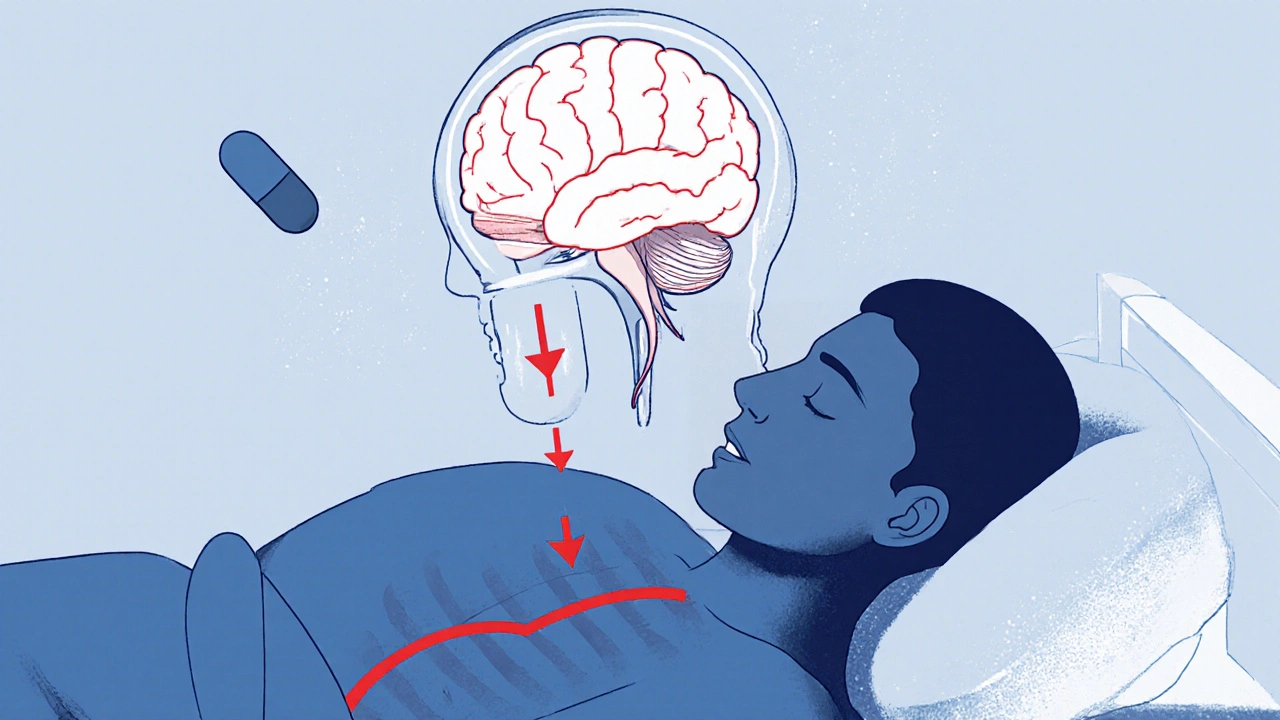
When you sleep, your body should keep getting enough oxygen—no matter how deep you’re dozing. But for many people, nighttime hypoxia, a drop in blood oxygen levels during sleep. Also known as nocturnal hypoxemia, it happens when breathing slows or stops just enough to starve your tissues of oxygen. This isn’t just about feeling tired in the morning. It’s a silent stress test on your heart, brain, and lungs—and it’s more common than you think.
Most cases link to sleep apnea, a condition where breathing repeatedly pauses during sleep. These pauses can last 10 seconds or longer, and happen dozens of times an hour. Your body doesn’t wake you up fully, but it does jerk you out of deep sleep enough to restart breathing—leaving you exhausted without knowing why. Over time, your blood oxygen levels dip below 90%, sometimes even below 80%. That’s not normal. That’s your body screaming for help.
And it’s not just apnea. low blood oxygen, a measurable drop in oxygen saturation in the bloodstream can also come from COPD, obesity, heart failure, or even high-altitude sleeping. If you snore loudly, wake up gasping, or feel foggy all day even after 8 hours in bed, your oxygen levels might be dipping too low. Simple tools like pulse oximeters—those little clips you wear on your finger—can catch this at home. No doctor visit needed to start looking.
What’s scary is how often this goes ignored. People think snoring is normal. They blame fatigue on stress or age. But nighttime hypoxia doesn’t just make you grumpy—it raises your risk of high blood pressure, irregular heartbeats, stroke, and even memory loss. The longer it goes untreated, the more damage piles up. And the fix? Often simple: a CPAP machine, weight loss, changing sleep position, or treating the root cause. But you can’t fix what you don’t measure.
Below, you’ll find real-world guides on how to recognize the signs, what tests actually matter, how to interpret your oxygen readings, and what treatments work—without the fluff. These aren’t theoretical articles. They’re from people who’ve been there: tracking their oxygen levels, adjusting meds, fighting misdiagnoses, and finally getting their sleep—and their health—back.
- November 15, 2025
- Comments 14
- Health and Wellness