Opioid Respiratory Depression: What It Is, How It Happens, and How to Stay Safe
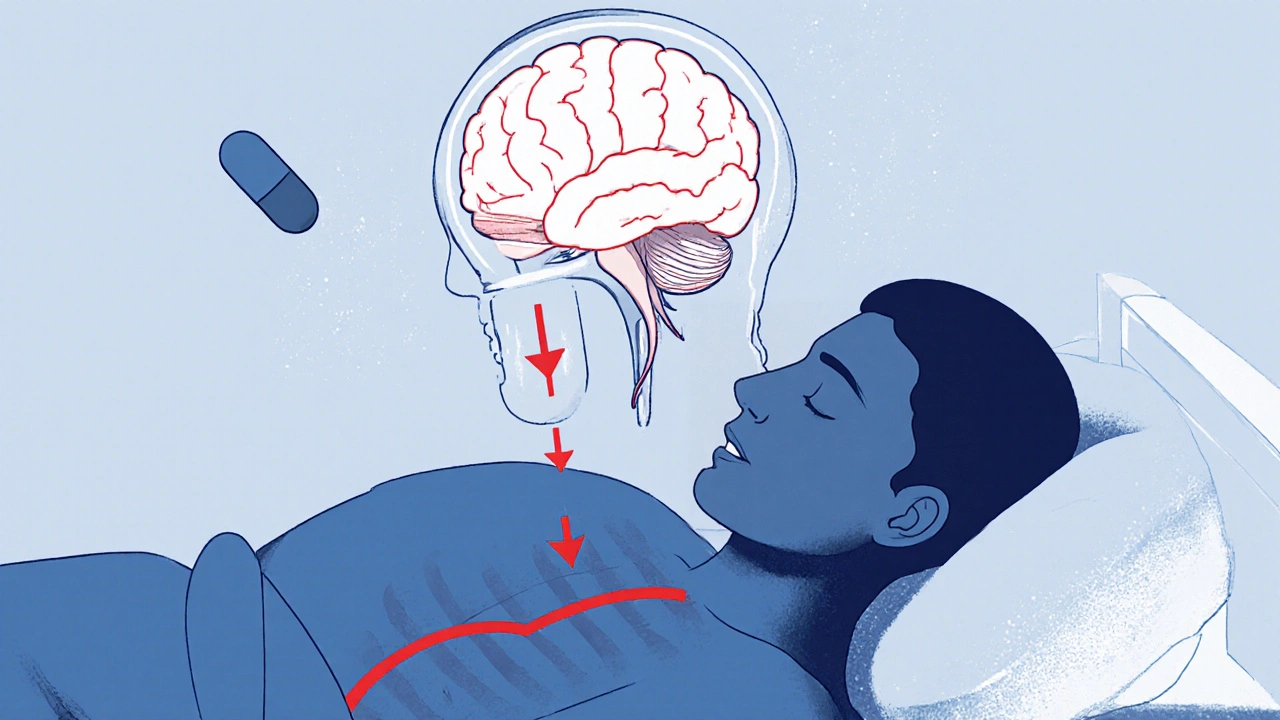
When someone takes too much of an opioid—whether it’s prescription painkillers like oxycodone, hydrocodone, or illegal drugs like heroin—their breathing can slow down dangerously. This is called opioid respiratory depression, a condition where opioids suppress the brain’s drive to breathe. It’s not just a side effect—it’s the #1 cause of death in opioid overdoses. You don’t need to take a huge dose for this to happen. Even people using their prescribed meds can slip into it, especially if they mix opioids with alcohol, benzodiazepines, or sleep aids.
Naloxone, a fast-acting drug that reverses opioid effects is the first line of defense. It’s not a cure, but it buys time—enough to get emergency help. Many families now keep naloxone on hand, just like an EpiPen. Respiratory failure, when breathing stops completely can follow if naloxone isn’t given quickly. It doesn’t always look like someone is passed out. Early signs include slow, shallow breaths, blue lips, gurgling sounds, or unresponsiveness. These aren’t signs of being "just sleepy"—they’re red flags.
People on long-term opioid therapy for chronic pain are at higher risk, especially if their dose gets changed or if they’ve gone without opioids for a while and then restart. Older adults, those with sleep apnea, or people with lung problems are also more vulnerable. It’s not about being "addicted"—it’s about how opioids interact with the brainstem, the part that controls automatic breathing. Even someone taking meds exactly as prescribed can experience this under the wrong conditions.
The good news? This isn’t inevitable. Knowing the signs, keeping naloxone nearby, and avoiding mixing drugs cuts the risk dramatically. If you or someone you care for uses opioids, talk to your doctor about naloxone. Ask if your dose is still right for you. And if you ever see someone struggling to breathe after taking an opioid—don’t wait. Call 911. Give naloxone. Start rescue breathing if you know how. Minutes matter.
Below, you’ll find real-world guides on how to spot early warning signs, how to use naloxone correctly, what drug combinations to avoid, and how to protect loved ones who rely on opioid medications. These aren’t theoretical discussions—they’re practical steps taken by families who’ve been through it.
- November 15, 2025
- Comments 14
- Health and Wellness