Topical Steroid Withdrawal: Symptoms, Causes, and What to Do Next
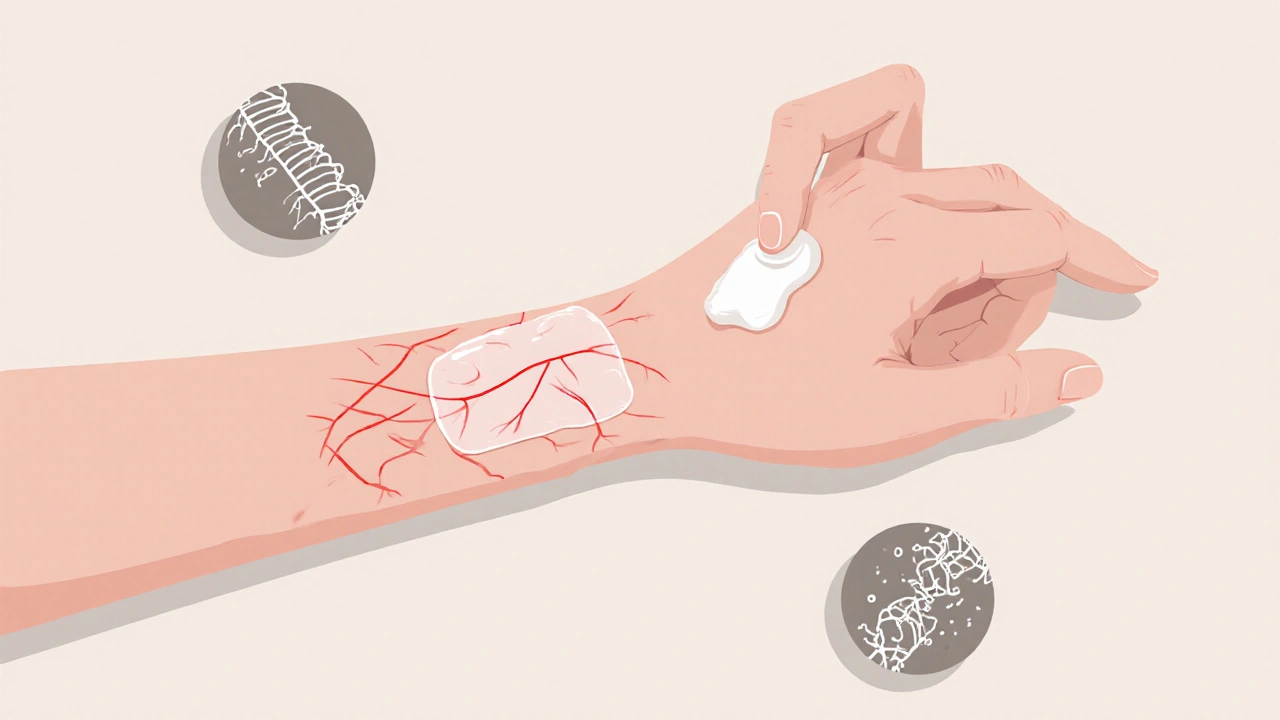
When you stop using topical steroid creams after long-term use, your skin might react badly—burning, redness, peeling, or intense itching. This isn’t just a rash. It’s topical steroid withdrawal, a condition that occurs when the skin becomes dependent on corticosteroid creams and rebounds after stopping them. Also known as red skin syndrome, it’s not rare, but it’s often missed by doctors who don’t recognize the pattern.
This isn’t an allergic reaction. It’s a physiological response. Your skin’s natural ability to regulate inflammation gets suppressed over time by daily steroid use, especially on the face, genitals, or folds like armpits and groin. When you quit, your body overcompensates. The inflammation doesn’t disappear—it explodes. Some people see symptoms within days. Others wait weeks. It can last months. And it’s not just about the skin. Many report sleep loss, anxiety, and even depression during this phase.
What makes it worse? Stopping cold turkey. Using strong steroids like clobetasol for months without medical oversight. Thinking "less is better" when you’re told to taper. And believing that if your skin looks better on steroids, it must be healing. It’s not. It’s masking. The real issue? Most people don’t know they’re at risk until it’s already happening. You might’ve used hydrocortisone for eczema, psoriasis, or a persistent itch—maybe for years—and assumed it was safe because it was "over-the-counter." But even mild steroids can cause dependence if used too often or too long.
There’s no FDA-approved treatment for topical steroid withdrawal. But that doesn’t mean nothing helps. People find relief through gentle skincare—no scrubs, no fragrances, no alcohol-based products. Cool compresses. Moisturizers with ceramides. Avoiding heat and sweat. Some use non-steroidal anti-inflammatories like pimecrolimus under doctor supervision. Others wait it out, knowing time is the only real cure. And while some doctors still dismiss it as "psychosomatic," patient groups and dermatologists who specialize in this are pushing for better recognition.
What you’ll find in the posts below isn’t theory. It’s real-world guidance. You’ll see how people managed withdrawal symptoms while avoiding common mistakes. You’ll learn why certain moisturizers work better than others. You’ll understand how to talk to your doctor about tapering safely. And you’ll see how medications like gabapentin and antihistamines sometimes help with nerve-related itching, even if they don’t fix the root cause. There’s also advice on spotting when a flare is withdrawal versus a new infection, and how to protect your skin while your body recalibrates.
- November 28, 2025
- Comments 10
- Health and Wellness