Putting together multiple sedating medications might seem like a simple fix for sleep problems, anxiety, or chronic pain-but it’s one of the most dangerous things people do without realizing it. Every year in the U.S., over 1.3 million emergency room visits happen because of bad drug combinations, and nearly 128,000 people die from prescription drug-related causes. The biggest killers? When opioids, benzodiazepines, alcohol, or sleep aids are mixed together. These aren’t rare accidents. They’re predictable, preventable tragedies-and they’re happening right now to people you know.
How Sedating Medications Work Together (And Why It’s So Dangerous)
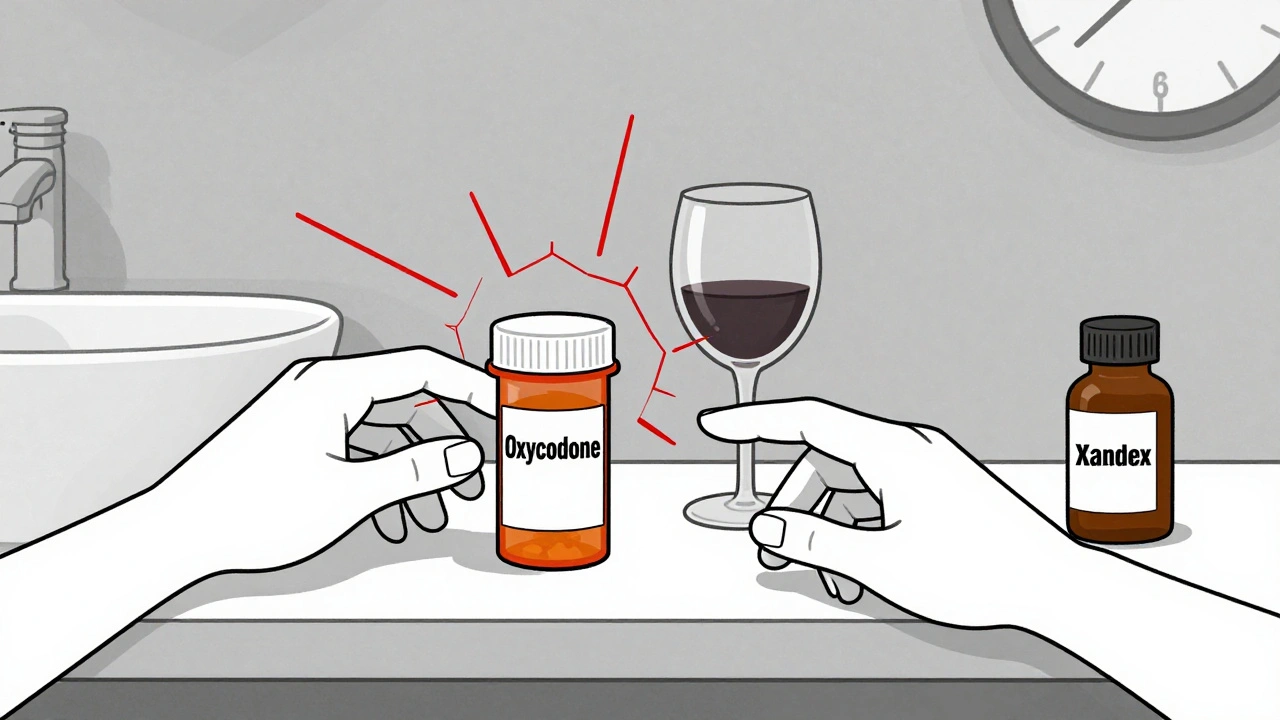
Most sedating drugs-whether they’re prescription opioids like oxycodone, benzodiazepines like Xanax or Valium, sleep pills like Ambien, or even over-the-counter antihistamines-work by slowing down your brain. They boost a chemical called GABA, which tells your nervous system to calm down. That’s fine if you’re taking one. But when you mix two or more, they don’t just add up. They multiply. Think of it like stacking weights. One weight might make you drowsy. Two weights make you really sleepy. But three? Suddenly, your breathing slows to a dangerous crawl. Your brain stops telling your lungs to work. Oxygen drops. Your heart struggles. And you don’t even realize it’s happening. A 2017 study in JAMA Internal Medicine found people taking both opioids and benzodiazepines had a 154% higher risk of overdose than those taking opioids alone. That’s not a small bump. That’s a wall. The FDA warned about this in 2016-and still, in 2020, 16% of opioid-related overdose deaths also involved benzodiazepines.The Deadliest Combinations (And What They Do to Your Body)
Not all combinations are equal. Some are worse than others. Here are the most dangerous ones, based on real-world data:- Opioids + Benzodiazepines: This is the #1 killer. Opioids shut down your brainstem’s breathing control. Benzodiazepines make that shutdown faster and deeper. Together, they’re responsible for about 30% of all prescription drug deaths. A 2019 study showed people on both had a 3.86 times higher risk of fatal overdose.
- Alcohol + Any Sedative: Alcohol is a sedative too. Mixing it with Ambien, Valium, or even a low-dose sleep aid can reduce reaction time by 70%-more than double the effect of either alone. It’s why so many people wake up with bruises, broken bones, or no memory of how they got there.
- SSRIs + MAOIs: These are antidepressants. Taken together, they can trigger serotonin syndrome-a life-threatening surge of serotonin that causes high fever, seizures, muscle rigidity, and heart rhythm problems. About 14-16% of cases are fatal if not treated fast.
- Older Adults + Multiple Sedatives: The American Geriatrics Society lists 19 dangerous combinations to avoid in people over 65. Why? Because aging slows how your body clears drugs. One pill might be fine. Three? You’re at 50% higher risk of falling. And falls in older adults often lead to broken hips, long-term disability, or death.
Warning Signs You’re in Danger
You don’t need to wait for an overdose to realize something’s wrong. These signs mean you or someone you care about is in immediate danger:- Breathing fewer than 12 times per minute
- Blue lips or fingertips
- Unresponsiveness-even when shaken or called loudly
- Extreme confusion or inability to stay awake
- Gurgling sounds when breathing (a sign of airway blockage)
Why Doctors Miss These Risks
You’d think doctors would catch this. But here’s the truth: most don’t. A 2020 study found that only 17.3% of dangerous drug combinations triggered alerts in electronic health records. That means your doctor’s computer didn’t even warn them. Many providers still don’t ask about over-the-counter meds, supplements, or alcohol use. A patient might say they’re on oxycodone and Xanax-and forget to mention they drink two glasses of wine every night. Or they take diphenhydramine (Benadryl) for allergies, not realizing it’s a powerful sedative. The Beers Criteria, used by doctors to guide safe prescribing for older adults, says no one over 65 should take more than 5mg of diazepam (Valium) per day. But a 2023 report showed 35% of seniors still take inappropriate sedatives. Women are even more likely-41% vs. 27% of men.What You Can Do to Stay Safe
You don’t have to accept this risk. Here’s how to protect yourself:- Keep a full list of everything you take. Not just prescriptions. Include supplements, herbal teas, sleep aids, and alcohol. Bring it to every appointment.
- Ask your doctor: “Is this safe with my other meds?” Don’t assume they know. Be specific: “I take Ambien and ibuprofen-what about this new painkiller?”
- Know your morphine milligram equivalents (MME). If you’re on opioids, your daily dose matters. The CDC says staying under 50 MME per day reduces overdose risk. Above 90 MME? Risk spikes dramatically.
- Never mix alcohol with sedatives. Not even one drink. Not even on “special occasions.” The risk isn’t worth it.
- Get a medication review every 3 months if you’re over 65 or taking three or more sedating drugs. The START criteria say this is non-negotiable.
- Don’t get prescriptions from multiple doctors. A 2022 study found 42% of people who overdosed on sedatives got prescriptions from three or more doctors in six months. That’s called “doctor shopping”-and it’s how people accidentally kill themselves.

There’s Hope-Safer Alternatives Exist
You don’t have to live with anxiety, insomnia, or pain using dangerous drugs. There are safer options:- For anxiety: Cognitive behavioral therapy (CBT) works as well as benzodiazepines-with no risk of addiction.
- For sleep: Sleep hygiene, melatonin (short-term), and CBT for insomnia (CBT-I) are more effective long-term than Ambien.
- For pain: Physical therapy, acupuncture, and non-opioid pain relievers like gabapentin or duloxetine can be just as effective without the respiratory risk.
Final Reality Check
Some people say, “My doctor said it was fine.” But doctors aren’t mind readers. They rely on what you tell them. If you don’t mention the wine, the Benadryl, or the melatonin gummies, they can’t protect you. This isn’t about being perfect. It’s about being aware. You don’t need to quit all your meds overnight. But you do need to ask the hard questions. You need to know what you’re mixing. And you need to understand that what feels like a small choice-like having a glass of wine with your sleeping pill-could be the one that ends your life. The data doesn’t lie. The warnings aren’t hypothetical. The deaths are real. Your life isn’t worth the risk.Can I just take one less pill to stay safe?
Not always. Stopping sedatives suddenly can be dangerous, especially benzodiazepines or opioids, which can cause seizures or severe withdrawal. The safest approach is to work with your doctor to reduce one medication at a time-usually by 10-25% every 1-2 weeks. Never adjust doses on your own.
Are natural sleep aids like melatonin or valerian root safe to mix with prescription sedatives?
No. Even “natural” supplements can be sedating. Melatonin may seem mild, but when combined with Ambien or a benzodiazepine, it can deepen drowsiness and slow breathing. Valerian root has similar effects. Always treat supplements like medications-they interact, too.
I’m on opioids for chronic pain. Can I ever take a benzodiazepine for anxiety?
The CDC and FDA strongly advise against it. If you’re already on opioids, your doctor should first try non-sedating treatments for anxiety-like SSRIs or CBT. If a benzodiazepine is absolutely necessary, it should only be for a very short time, at the lowest possible dose, with daily monitoring. Most experts say: avoid it entirely.
What should I do if I suspect someone is overdosing on sedatives?
Call emergency services immediately. Don’t wait. Try to keep them awake and in a recovery position (on their side). If you have naloxone (Narcan), use it-though it only reverses opioids, not benzodiazepines or alcohol. Even if they seem to wake up, they still need medical care. Respiratory depression can return hours later.
Why don’t pharmacies warn me when I pick up these meds?
Many do-but not always. Pharmacists can flag dangerous combinations, but they depend on complete records. If your prescriptions come from different doctors or pharmacies, the system might not connect the dots. Always ask your pharmacist: “Is this safe with my other meds?” Don’t assume they know.
Are there any safe combinations of sedating medications?
Only under strict medical supervision. A small number of patients with severe, treatment-resistant conditions may be on carefully managed combinations-but this is rare and requires daily monitoring, frequent lab tests, and specialist oversight. For 99% of people, the risks far outweigh any perceived benefit.
Next Steps: What to Do Today
1. Grab your pill bottle or medication list. Write down everything you take, including supplements and alcohol use.2. Call your doctor or pharmacist. Ask: “Are any of these medications dangerous to take together?”
3. If you’re on opioids and benzodiazepines, ask if you can switch to a non-sedating alternative.
4. If you’re over 65 and taking three or more sedatives, request a medication review within the next 30 days.
5. Tell someone you trust about your meds. They might notice warning signs before you do. This isn’t about fear. It’s about control. You have the power to ask questions, make changes, and protect your life. Start today.


Comments (8)
It’s wild how we treat our bodies like a DIY chemistry set, right? We’ll mix pills like cocktail ingredients and call it ‘self-care.’
But the brain isn’t a Slack channel-you can’t just ping GABA and expect a polite reply.
They’re lying. This whole thing is a Big Pharma scam to push you into therapy and make you buy expensive ‘alternatives’ that don’t work.
My cousin took Xanax and oxycodone for years-he’s fine. They just want you scared so you’ll take their SSRIs instead.
Of course you die if you mix meds-you’re not a robot, you’re a human who can’t even read a label.
India has 1.4 billion people and zero opioid epidemics because we don’t treat medicine like candy.
Stop pretending this is a ‘system failure.’ It’s just dumb.
I’ve been sitting with this for hours… and I keep thinking: we’ve built a system that rewards silence, not safety.
Doctors are overwhelmed, pharmacies are under-resourced, patients are terrified to speak up-and so we all just… keep taking the pills.
What if the real tragedy isn’t the combination-but the fact that we’ve normalized this slow, quiet surrender?
It’s not just medical-it’s cultural. We’ve forgotten how to ask for help without shame.
And yet, here we are, scrolling through lists of dangers, nodding along… and still not calling our doctor.
Maybe the first step isn’t changing the meds-it’s changing how we talk about them.
Not with fear.
Not with blame.
But with tenderness.
Because someone reading this right now? They’re not being reckless.
They’re exhausted.
And they just want to sleep.
And that’s not a crime.
It’s a cry.
And we’re the ones who’ve trained them to whisper it.
Bro, I take Ambien and a beer every night. I’m fine. You’re overreacting.
My buddy does it with oxycodone too. He’s got a dog and a job. What’s the big deal?
You’re not alone. I was on three sedatives last year. I didn’t realize how bad it was until my mom noticed I stopped laughing.
One conversation with my pharmacist changed everything.
You can heal without hitting rock bottom.
Start today. One pill. One question. One breath.
You’ve got this.
Just wanted to add: if you’re on opioids, ask about naloxone. It’s free at most pharmacies and saves lives.
And if you’re over 65? Ask your doctor about the Beers Criteria. It’s not a suggestion-it’s a lifeline.
Also, melatonin isn’t harmless. Even 5mg with Ambien can crash your breathing. I’ve seen it.
Keep that list. Bring it to every appointment. Even if they don’t ask.
Your life isn’t a guesswork experiment.
Of course Western medicine is broken-because it’s run by white men who don’t understand real pain.
India uses Ayurveda and still has lower opioid deaths-because we treat the soul, not just the synapse.
Stop importing American fear into our homes.
My grandmother never took pills-she drank turmeric milk and slept like a baby.
Why are we abandoning wisdom for pills and algorithms?