Getting a prescription wrong because of a poorly documented drug allergy isn’t just a mistake-it can be life-threatening. Every year, thousands of people end up in emergency rooms because someone, somewhere, wrote down "penicillin allergy" without saying what actually happened. Was it a rash? Hives? Trouble breathing? Or did they just feel nauseous after taking it once? These details matter. And if they’re missing, your medical record might be doing more harm than good.
Why Vague Allergy Notes Are Dangerous
Most people say, "I’m allergic to penicillin"-and that’s where the problem starts. Studies show that 90 to 95% of people who claim a penicillin allergy aren’t actually allergic when tested. But if your chart just says "penicillin allergy," doctors will avoid the drug entirely-even if it’s the best, cheapest, or only effective treatment for your infection.
That’s not just inconvenient. It means you might get a stronger, more expensive antibiotic with worse side effects. You could end up with a longer hospital stay. Or worse, you could get a drug that’s more likely to cause a different kind of reaction. Incomplete allergy records contribute to about 6.5% of all medication errors, according to the Journal of the American Medical Informatics Association.
And it’s not just penicillin. People say "sulfa allergy" when they mean they got a rash from Bactrim. Or "aspirin allergy" when they just had an upset stomach. These vague labels stick in your record forever-and they change how you’re treated.
What Your Medical Record Needs to Include
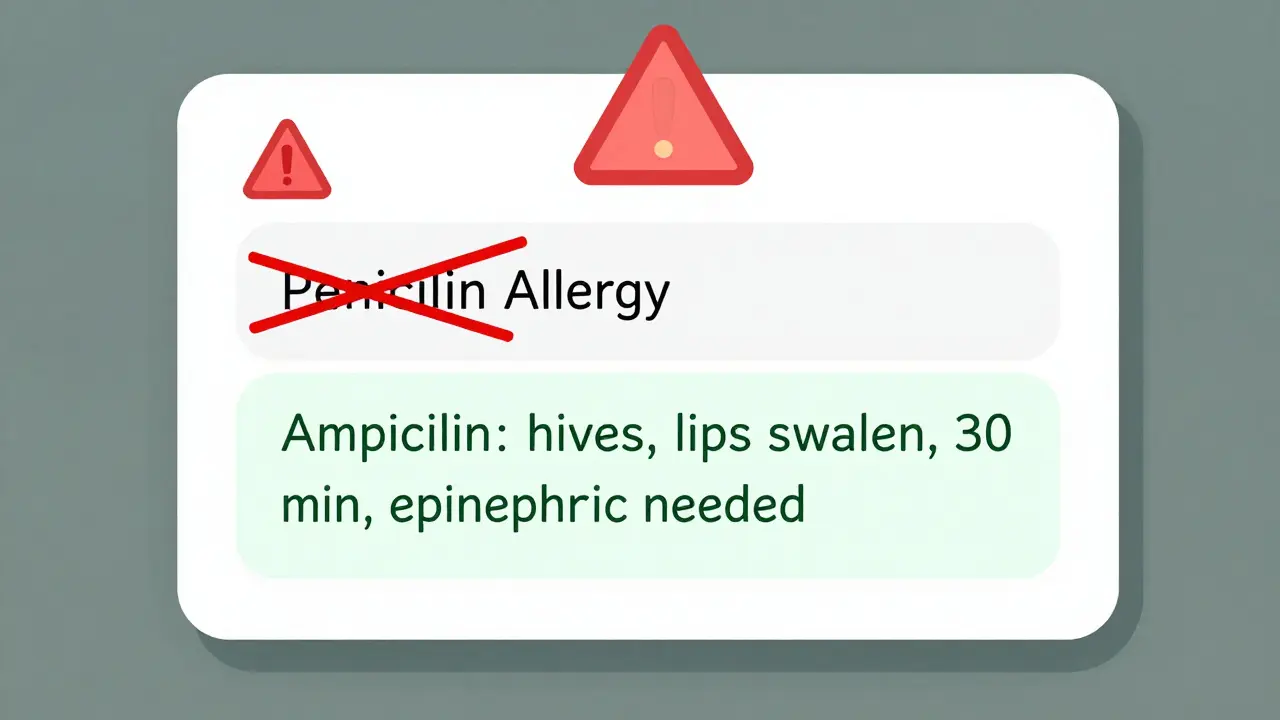
Safe documentation isn’t about checking a box. It’s about telling the full story. The U.S. Centers for Medicare & Medicaid Services (CMS) and The Joint Commission require that your allergy information includes four key things:
- The exact drug name-use the generic name, not the brand. Write "ampicillin," not "Amoxil." Write "ibuprofen," not "Advil."
- The reaction-what happened? Rash? Swelling? Vomiting? Low blood pressure? Anaphylaxis?
- The severity-was it mild, moderate, or life-threatening?
- The timing-when did the reaction happen? Minutes after taking it? Days later?
For example: "Ampicillin, 2018. Developed hives and swelling of lips within 30 minutes of dose. Required epinephrine. Diagnosed as IgE-mediated reaction."
That’s specific. That’s useful. That tells a doctor: "Don’t give this drug, ever. And if they accidentally do, be ready for an emergency."
On the flip side, if you had nausea after taking ibuprofen once and never had another issue? That’s not an allergy. That’s an intolerance. Write: "Ibuprofen: mild nausea, resolved without treatment. No rash, no breathing issues." That gives your doctor room to consider alternatives if needed.
How EHRs Are Changing the Game
Most doctors now use electronic health records (EHRs)-systems like Epic, Cerner, or Meditech. These aren’t just digital notebooks. They’re smart systems that can warn doctors before they prescribe something dangerous.
But only if the data is entered right. CMS requires that more than 80% of patients have their allergy status recorded as structured data-not just scribbled in a free-text note. That means the system must recognize "penicillin" as a drug, "hives" as a reaction, and "severe" as a severity level.
When done correctly, these systems cut allergy-related errors by up to 55%. They can flag conflicts before the prescription is even printed. They can suggest safer alternatives. They can even remind your doctor to ask you again if your allergy status has changed.
And here’s the catch: if you say "no known allergies," your record must say that clearly. Not "NKDA" in tiny letters. Not a checkbox left blank. It must be a full, unambiguous statement: "No known drug allergies." That’s a legal requirement under CMS rules.
What You Can Do to Protect Yourself
You’re not just a patient. You’re the most important person in your own medical record. Here’s how to make sure your allergy info is accurate:
- Review your record-ask for a copy of your allergy list at your next visit. Don’t assume it’s right.
- Clarify old labels-if you wrote "allergic to penicillin" years ago, ask: "What exactly happened?" If it was just a stomachache, update it.
- Bring a list-write down every drug you’ve ever reacted to, with details. Bring it to appointments.
- Ask about testing-if you think you’re allergic to penicillin but aren’t sure, ask your doctor about a skin test. Many people are mislabeled.
- Use the Drug Allergy History Tool-some clinics use this simple questionnaire to help patients recall reactions accurately. Ask if they offer it.
A 2018 study at Massachusetts General Hospital found that after using a structured interview, 61% of patients needed changes to their allergy records. Over 200 vague entries were cleaned up. That’s not a small fix-that’s a safety revolution.
Don’t Assume Your Allergy Is Permanent
Drug allergies can fade. Many people outgrow penicillin allergies within 10 years. Others never had one to begin with. If you haven’t taken a drug in 5+ years and never had a reaction since, talk to your doctor about whether you still need to avoid it.
Getting tested isn’t just for the curious-it’s for the safe. A simple skin test or oral challenge can clear up confusion and open up better treatment options. And if you’re cleared? Make sure your record reflects that change.
What Happens If You Don’t Document Properly?
Healthcare facilities can lose their Medicare certification if they fail to meet documentation standards. That’s how seriously this is taken. But beyond regulations, the real cost is human.
The Institute of Medicine estimated in 2006 that better allergy documentation could prevent 1.3 million injuries and 7,000 deaths each year in the U.S. alone. That’s not a statistic-it’s your neighbor, your parent, your friend.
And it’s not just hospitals. Pharmacies, urgent cares, even telehealth providers rely on your record. If your allergy info is missing or wrong when you’re seen remotely, they can’t make safe choices.
The Future Is Clearer-But Only If You Help
By the end of 2023, all certified EHRs in the U.S. must use the FHIR standard to share allergy data across systems. That means if you go to a new clinic, your allergy info should follow you-accurately and safely.
By 2025, patients will be able to update their own allergy records through patient portals. Imagine being able to add a reaction right after your appointment, or remove an old label you’ve since clarified.
And AI is coming. New tools can scan your doctor’s notes and pull out hidden allergy clues. One study showed 85% accuracy in finding drug-reaction pairs buried in free text. But these tools only work if the data is detailed enough to find.
So your job isn’t done when you tell your doctor. Your job is to make sure that information gets recorded right-and stays right.
Final Thought: Your Record Is Your Shield
Medication errors are preventable. But only if the right information is in the right place. A vague allergy note is like a broken alarm system-it gives you a false sense of safety.
Be specific. Be honest. Be persistent. If your doctor writes "penicillin allergy" without details, say: "Can you add what happened?" If your record says "no known allergies" but you’ve had reactions, speak up. You’re not being difficult-you’re saving your own life.
What if I don’t remember exactly what happened during my reaction?
It’s okay not to remember every detail. Start with what you do know-like "I broke out in a rash after taking amoxicillin." Then ask your doctor if they can help you trace it back. Many clinics now use structured questionnaires to guide patients through recalling reactions. Even partial info is better than nothing. If you’re unsure, don’t guess. Write "unclear reaction to amoxicillin" and ask to follow up later.
Can I remove an allergy from my record if I think it’s wrong?
Yes, but you need evidence. If you’ve taken the drug since without issue, or if you’ve had a formal allergy test that cleared you, bring that documentation to your doctor. They can update your record with a note like: "Previously documented penicillin allergy. Re-evaluated in 2024. No reaction confirmed. Allergy status removed." Don’t assume your record updates itself-ask for it.
Does a family history of drug allergies mean I have them too?
No. Drug allergies are not inherited like eye color. Just because your mom is allergic to sulfa doesn’t mean you are. Your reaction is based on your own immune response. Don’t list family allergies on your record unless you personally had a reaction. Adding someone else’s history can lead to dangerous misdiagnoses.
What if my doctor doesn’t update my record after I tell them about a reaction?
Politely insist. Say: "I need this added to my official record so future providers know." If they refuse, ask to speak to the office manager or request a copy of your record to update it yourself. You have the right to accurate medical documentation. If you’re still blocked, contact your health plan’s patient advocate. Your safety is non-negotiable.
Are over-the-counter drugs like ibuprofen or aspirin really dangerous if I’m allergic?
Yes. Many people think only prescription drugs matter. But reactions to OTC painkillers like ibuprofen, naproxen, or aspirin can be just as serious. If you’ve had swelling, trouble breathing, or hives after taking them, document it. These drugs are common in hospitals and ERs. If your record doesn’t show a reaction, you could be given one in an emergency.
Can I carry a card or app with my allergy info?
Yes, and you should. But don’t rely on it alone. A wallet card or phone app is a backup, not a replacement. Emergency responders may not check your phone. Your official medical record must still be accurate. Use the card as a reminder to update your chart, not as your primary safety net.

Comments (10)
Been there. Thought I was allergic to penicillin because I got a rash after one dose in college. Turns out it was just a viral thing. Got tested last year-zero allergy. My doctor was shocked I’d been avoiding half the antibiotics for 12 years. Seriously, if you’re unsure, get tested. It’s a 15-minute skin test and could save you from a nightmare antibiotic later.
I just asked my mom to review her record after reading this-she’s had ‘sulfa allergy’ since the 90s because she got a rash from Bactrim. Turns out she took it once for a UTI and it faded in a day. No swelling, no breathing issues. She’s been avoiding all sulfa drugs since, including diabetes meds. Now she’s gonna get retested. This post is a game-changer.
Structural documentation of allergies is non-negotiable in FHIR-compliant EHRs. The SNOMED CT codes for drug reactions (e.g., 414287005 for urticaria, 24420004 for anaphylaxis) must be mapped to the allergy section with appropriate severity modifiers (mild/moderate/severe) and temporal context. Without this, clinical decision support systems are blind. We’re seeing 40% reduction in ADEs in our clinic since enforcing structured entry. It’s not just best practice-it’s clinical infrastructure.
My sister nearly died because her chart said ‘penicillin allergy’ but didn’t say it was just a rash from 1998. They gave her vancomycin instead-she went into renal failure. This isn’t paperwork. This is life or death. If your doctor doesn’t update your record after you tell them, fire them. I’m not kidding. Your record is your lifeline. Stop being polite. Be loud. Be relentless. I lost a year of my life because someone checked a box and didn’t ask a question.
OMG I just realized I’ve been writing ‘NKDA’ on every form since high school. But I broke out in hives after ibuprofen in 2017. I never told anyone because I thought it was ‘just a reaction’ and not an ‘allergy.’ I’m calling my doctor tomorrow to fix this. And yes, I’m bringing my old ER note with the scribbled ‘urticaria’ on it. This post just gave me a panic attack in the best way possible.
Why do we even let patients document their own allergies?!??! You think some guy who got a stomachache after Advil in 2005 knows the difference between an intolerance and an IgE-mediated anaphylaxis?!?!? This is why American healthcare is a dumpster fire. Let the damn doctors decide what goes in the chart. I’m sick of patients acting like they’re immunologists. 🤦♂️💥
In India, we often see patients who’ve been told they’re allergic to ‘antibiotics’ because they had diarrhea after one course. No details. No clarity. We’ve started using a simple 5-question tool at our clinic: ‘What drug? What happened? When? How bad? Did it happen again?’ It’s cut our misdiagnoses by 60%. This isn’t just a U.S. problem-it’s global. Documentation is equity.
Just updated my portal. Changed ‘penicillin allergy’ to ‘Ampicillin, 2019: mild rash on chest, resolved in 48 hrs, no swelling or breathing issues.’ I also added ‘No reaction to cephalexin in 2022.’ Took me 5 minutes. My doctor’s office confirmed it was updated. Small effort. Huge impact. If you’re reading this and have a vague allergy in your record-do this. Now.
As a Canadian physician who has worked across both public and private systems, I can attest that the granularity of allergy documentation is the most underappreciated pillar of patient safety. The absence of structured data not only impedes clinical decision-making but also creates cascading inefficiencies in inter-provincial and cross-border care. I urge all patients to treat their allergy record with the same reverence as their passport-because, in truth, it may well be the document that saves your life during a medical emergency abroad.
Just read David’s comment above. Dude, you’re missing the point. Patients are the only ones who know what happened to their own bodies. Doctors forget, records get corrupted, and EHRs are terrible at interpreting free text. The system needs patient input to function. It’s not about ‘letting patients be immunologists’-it’s about empowering the only person who actually lived the reaction to help fix the system. If you think this is chaos, you’ve never tried to trace a 20-year-old allergy note in Epic.