Every year, thousands of children end up in emergency rooms because of a simple mistake: the wrong amount of medicine. Not because parents are careless, but because the system is stacked against them. In pediatric emergencies, medication errors happen more than twice as often as in adults. One study found 31% of pediatric medication orders contain mistakes - compared to just 13% in adults. And in real life, those numbers translate to kids getting 10 times too much acetaminophen, or parents mixing up milligrams with milliliters because the labels look the same.
Why Kids Are at Higher Risk
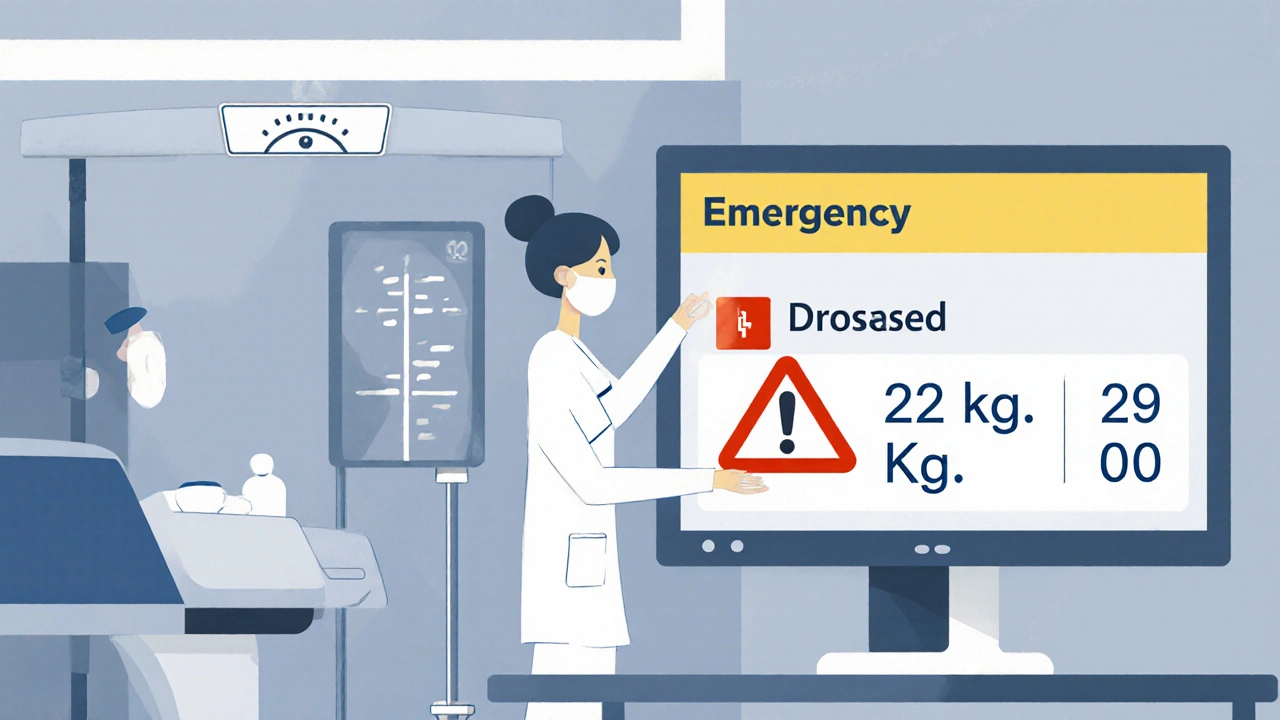
Adults get pills. Kids get liquids. That’s the first red flag. Liquid medications require precise dosing based on weight - not age, not size, not guesswork. A 10-kilogram toddler needs a completely different amount than a 30-kilogram child. One wrong decimal point, one misread label, and you’ve crossed the line from safe to dangerous. Weight-based dosing isn’t just complicated - it’s error-prone. Studies show that 10% to 31% of pediatric medication errors come from incorrect weight measurements. Sometimes the scale is broken. Sometimes the parent guesses. Sometimes the nurse writes down 20 kg instead of 22 kg - and the system doesn’t catch it. Then the computer calculates the dose: 15 mg/kg of amoxicillin becomes 300 mg instead of 330 mg. Sounds close, right? But in pediatrics, close isn’t good enough. Liquid formulations add another layer of confusion. There are different concentrations of children’s Tylenol: infant drops (80 mg/mL) and children’s suspension (160 mg/5 mL). Parents don’t know the difference. One Reddit user shared how they gave their 2-year-old 5 mL of children’s Tylenol thinking it was the same as infant drops. The child got nearly double the intended dose. The pediatrician called back an hour later. That’s not luck - that’s a near miss.The Most Common Mistakes - And What They Cost
The Child Health Patient Safety Organization tracked over 10,000 safety events in children’s hospitals between 2009 and 2022. Here’s what they found:- 13% of errors were wrong dose - the biggest category
- 4% were wrong medication - like giving amoxicillin instead of ibuprofen
- 3% were wrong rate or time - IV drip too fast, or a dose given 2 hours early
- 1% were wrong route - oral medicine given intravenously
Where the System Breaks Down
Emergency rooms are chaotic. Kids cry. Parents panic. Doctors rush. Nurses juggle ten things at once. In that environment, the smallest oversight becomes a disaster. Verbal orders are a major culprit. A doctor says, “Give 10 mg of morphine IV,” and the nurse writes it down. But the order isn’t checked. No pharmacist reviews it. No double-check happens. That’s how a child gets 100 mg instead of 10 mg. And then there’s the tech gap. Children’s hospitals have pediatric-specific EMRs that flag dangerous doses. They have built-in dosing calculators. They have pharmacy teams that verify every order. But community hospitals? Many still use generic adult-focused systems. A nurse types in “5 kg” and the system doesn’t scream “DANGER - THAT’S TOO HIGH.” It just calculates the dose. Quietly. Dangerously. Language barriers make it worse. Parents who don’t speak English fluently are 45% more likely to make dosing errors at home. One study showed Spanish-speaking families had 32% higher error rates than English-speaking ones - even when they got the same written instructions. Because the instructions weren’t translated well. Or the pictograms didn’t match their culture. Or the nurse didn’t use teach-back.What Works - Real Solutions From Real Hospitals
At Nationwide Children’s Hospital, they didn’t just train staff. They changed the system. And it worked. They started with three rules:- All pediatric doses must be calculated using weight in kilograms - no pounds allowed.
- High-alert medications like morphine, epinephrine, and insulin require two independent checks - one by a nurse, one by a pharmacist.
- Every order goes through real-time pharmacy verification before it’s given.
What Parents Can Do Right Now
You don’t need to be a nurse to keep your child safe. Here’s what you can do the next time you’re handed a medicine bottle:- Ask: “Is this dose based on my child’s weight?” If they say “yes,” ask them to show you the calculation.
- Ask: “What unit is this in? Milligrams or milliliters?” Many parents confuse the two.
- Ask: “Can you show me how to use this syringe?” Don’t trust the cap - trust the markings.
- Ask: “Can you have me repeat the dose back to you?” That’s teach-back. It’s not rude - it’s smart.
- Take a photo of the prescription label before you leave. Compare it later.
The Bigger Picture
This isn’t just about individual mistakes. It’s about broken systems. A child on Medicaid is 27% more likely to have a medication error than a child with private insurance. Kids in safety-net hospitals don’t have the same tech, the same pharmacy support, the same training. That’s not fair. That’s not right. The American Academy of Pediatrics is pushing for standardized pediatric medication error metrics by 2025. That’s a start. But until every ER - not just the big children’s hospitals - uses weight-based dosing calculators, requires double-checks, and trains staff in pediatric safety, these errors will keep happening. And until parents are given clear, simple, visual instructions - not dense medical jargon - they’ll keep making mistakes out of confusion, not carelessness. The good news? We know what works. We’ve seen it. We’ve measured it. We just need to make it standard - everywhere.What’s the most common pediatric medication error in emergency rooms?
The most common error is giving the wrong dose - often because of incorrect weight measurements or miscalculations in mg/kg. Studies show wrong dose errors make up 13% of all pediatric medication safety events, far more than giving the wrong medication or using the wrong route.
Why are liquid medications so risky for kids?
Liquid medications require precise volume measurements, and many have different concentrations. For example, infant Tylenol drops are 80 mg per mL, while children’s suspension is 160 mg per 5 mL. Parents often don’t realize the difference and give the wrong volume, leading to 10-fold overdoses. About 60-80% of home dosing errors involve liquid medications.
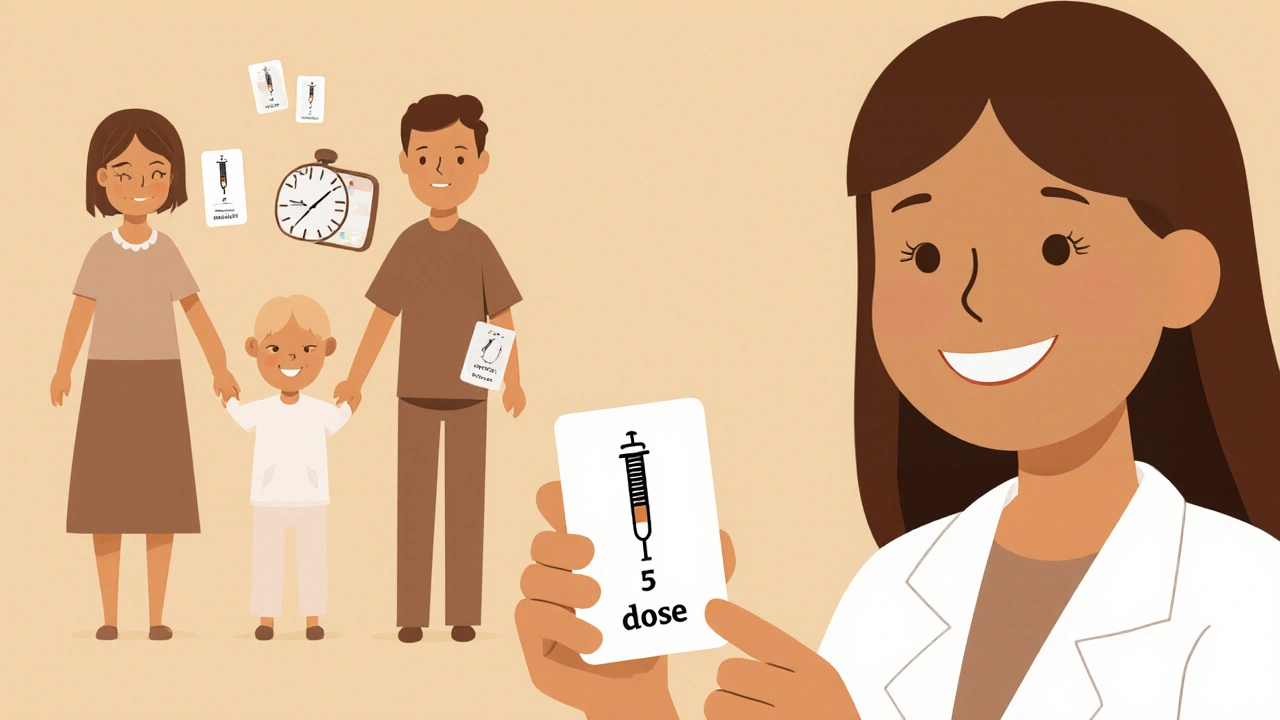
How can parents avoid dosing mistakes at home?
Always use the dosing syringe that comes with the medicine - never a kitchen spoon. Ask the provider to show you how to read the syringe. Write down the dose, time, and frequency. Use the teach-back method: repeat the instructions back to the nurse. And if you’re unsure, call your pediatrician before giving another dose.
Do emergency rooms have systems to prevent these errors?
Some do - especially children’s hospitals. They use weight-based dosing calculators in their electronic systems, require pharmacist verification, and double-check high-risk medications. But many community emergency rooms still use adult-focused software that doesn’t flag dangerous pediatric doses. This creates a dangerous gap in care.
Are medication errors in kids really that common?
Yes. Studies show 31% of pediatric medication orders contain errors - more than double the rate in adults. One in 10 parents of children with chronic illnesses make dosing mistakes at home. And because most errors go unreported, the real number is likely even higher.
What’s being done to fix this problem?
Hospitals like Nationwide Children’s have reduced harmful errors by 85% using double-check systems, pharmacist verification, and standardized protocols. Programs like MEDS have cut home dosing errors by using simple visual instructions and teach-back. The American Academy of Pediatrics is pushing for national standards by 2025. But progress is uneven - many hospitals still lack the tools or training.


Comments (13)
Every time I see a parent struggling with a syringe in the ER, I think about how we treat families like they’re supposed to be medical experts overnight. It’s not their fault. The system gives them a tiny bottle with tiny numbers and expects them to be precise under panic. We need better labeling, plain-language instructions, and mandatory teach-back - not just for safety, but for dignity.
This post is such a performative cry for sympathy. Of course kids get dosed wrong - parents are idiots. Stop pretending it’s the system’s fault. If you can’t read a label, maybe you shouldn’t be parenting. The real problem is people who think they deserve a medal just for not killing their kid.
In India, we use the same liquid medicines - but we’ve always had a culture of asking. Grandmas, neighbors, pharmacists - everyone chimes in. You don’t just take the bottle and go. You show it to three people. Maybe that’s not scalable, but it’s human. In the U.S., you’re handed a prescription like it’s a lottery ticket. No one checks. No one cares. We need that community layer back.
Let’s be real - this isn’t about medication. It’s about class. Poor families get rushed through ERs with poorly translated handouts. Rich families get pharmacists on speed dial and pediatric specialists who walk them through every drop. The fact that we call this a ‘safety issue’ instead of a moral failure is the real tragedy. We’ve normalized inequality as a logistical problem.
I’ve worked in pediatrics for 18 years. The most heartbreaking thing isn’t the overdose - it’s the parent who comes back weeks later, guilt-ridden, saying ‘I just didn’t know.’ They didn’t fail. The system did. We measure success by how many errors we catch, not how many we prevent. That’s backwards. Prevention should be the metric. Not damage control.
Parents are lazy. They don’t read. They don’t ask. They trust the nurse like she’s a wizard. Then they blame the hospital when their kid gets sick. I’ve seen it a hundred times. If you’re too tired to read the label, maybe you shouldn’t be giving medicine at all. This isn’t rocket science - it’s basic responsibility. Stop making excuses for incompetence.
Let me guess - you think a visual card and a 90-second teach-back is enough? That’s like handing someone a life jacket and calling it ‘safety training.’ The real solution? Ban liquid formulations for non-critical meds. Use tablets. Use patches. Use anything that doesn’t require a PhD in decimal math. And if you’re going to use liquids - make the syringes color-coded, size-specific, and impossible to misread. Stop treating parents like interns.
I’m a dad of two. I’ve held a syringe with shaking hands at 2 a.m. I’ve double-checked the label three times. I’ve called the pediatrician at midnight. And I still felt like I was gambling with my kid’s life. This isn’t about ‘being careful.’ It’s about design. If we can make a phone that doesn’t let you send a text without confirmation, we can make a medicine bottle that doesn’t let you overdose. We’re just choosing not to.
USA thinks it’s so advanced but can’t even get a child’s dose right? In India, even rickshaw drivers know how to mix antibiotics for kids. You have all the tech, all the money, all the doctors - and you still mess up because you think paperwork is enough. Wake up. Your system is broken. Not the parents.
I’m a nurse. I’ve caught 17 wrong doses in the last year. Not because I’m amazing - because we have double-check protocols. Every high-alert med? Two signatures. Every weight? Verified by two people. Every instruction? Taught back. It takes 90 extra seconds. But it saves lives. And guess what? The staff hates it at first. Then they realize they’re not going to be the one who killed a child. That’s the real win.
Most people don’t realize that the same syringe that comes with the medicine is calibrated for that specific concentration. If you use a different one - even from another bottle - you’re guessing. And the cap? It’s not a measuring tool. It’s a cap. I’ve seen parents use the cap to give 10 mL of syrup thinking it’s 5 mL because it looks half-full. That’s not negligence - that’s a design flaw. The FDA needs to mandate color-coded syringes and concentration labels in 12-point font. No more exceptions.
85% reduction at Nationwide? Cool. What’s the cost? How many staff hours? How many FTEs? Did they cut other services to fund it? Who’s paying for the pharmacy verification? Is this scalable? Or is this just a shiny demo for wealthy hospitals that don’t care about the real world? Real solutions don’t require miracles - they require budget lines.