Corticosteroid Infections: Risks, Signs, and How to Stay Safe
When you take corticosteroid infections, a serious risk that arises when long-term steroid use suppresses the body’s natural defenses. Also known as steroid-induced infections, this isn’t just a side effect—it’s a direct result of how these drugs work by calming inflammation at the cost of your immune system’s ability to fight back. Corticosteroids like prednisone, dexamethasone, and hydrocortisone are lifesavers for conditions like asthma, rheumatoid arthritis, and severe allergies. But every time you take them, especially for weeks or months, you’re quietly lowering your body’s guards against bacteria, viruses, and fungi.
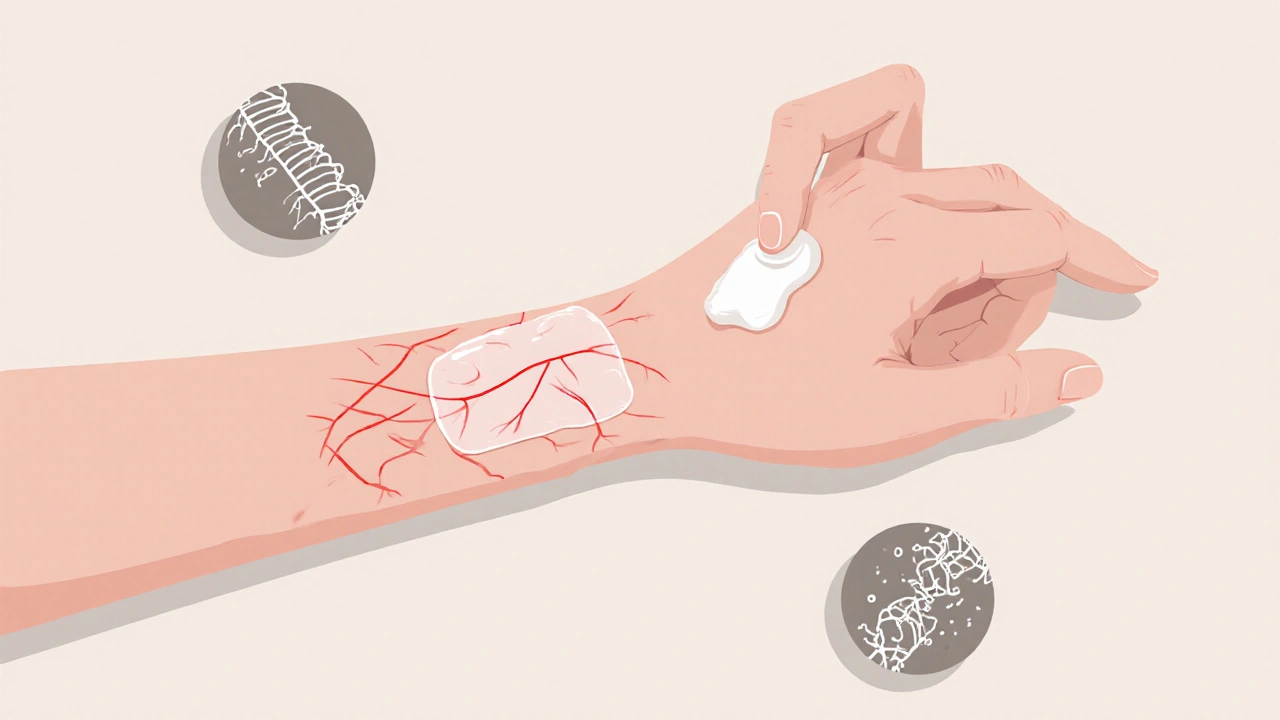
This isn’t theoretical. People on long-term steroids get pneumonia, skin abscesses, and even rare fungal infections like aspergillosis more often than others. The problem? These infections don’t always look like typical ones. No high fever. No obvious redness. Just a lingering cough, a slow-healing cut, or unexplained fatigue. That’s why immunosuppression, the intentional weakening of the immune response caused by corticosteroids is so sneaky. You might feel fine otherwise, but your body can’t mount a normal defense. And if you’re also on other immune-lowering drugs—like those for autoimmune diseases—the risk multiplies.
It’s not just about the dose. Duration matters just as much. Someone taking 5 mg of prednisone daily for six months has a much higher infection risk than someone who took a 7-day course. And it’s not just the drug itself—things like diabetes, smoking, or living in a nursing home add to the danger. That’s why steroid side effects, the full range of health impacts from corticosteroid use, including increased infection vulnerability need to be tracked closely. Your doctor should check for signs of infection at every visit, but you need to know what to watch for too.
Here’s what to look out for: a fever that won’t go away, even if it’s just 99.5°F; a sore throat that lingers beyond a few days; a wound that’s not healing after a week; or a rash that spreads instead of fading. Even a bad case of the flu can turn dangerous fast if you’re on steroids. And don’t ignore dental issues—oral thrush is one of the most common early signs. If you’re on long-term steroids, get your flu shot, stay up to date on vaccines, and avoid crowded places during cold and flu season.
There’s no magic fix, but you can reduce your risk. Never skip your doctor’s follow-ups. Don’t stop steroids suddenly—your body needs time to restart its own hormone production. And if you’re prescribed antibiotics or antifungals while on steroids, take them exactly as directed. Most importantly, speak up if something feels off. Too many people assume fatigue or a mild cough is just part of their condition, not a red flag.
The posts below give you real-world examples of how corticosteroid infections show up, how they’re mistaken for other problems, and what steps doctors and patients take to catch them early. You’ll find practical advice on monitoring your health, recognizing warning signs, and working with your care team to balance the benefits of these drugs with the risks they carry. This isn’t about avoiding steroids—it’s about using them safely, so they help without putting you in greater danger.
- November 28, 2025
- Comments 10
- Health and Wellness