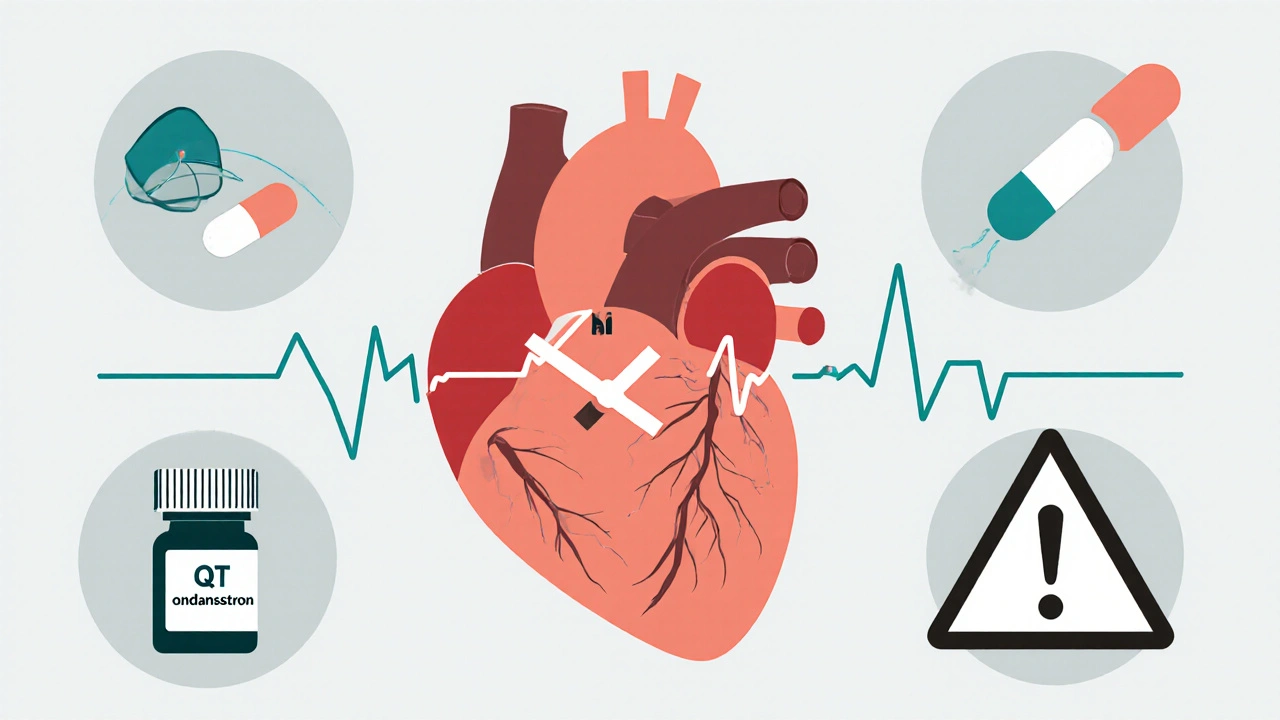
QTc Interval: What It Is, Why It Matters, and Which Medications Affect It
When your doctor talks about your QTc interval, a corrected measurement of the time your heart’s ventricles take to recharge between beats, often seen on an ECG. Also known as corrected QT interval, it’s not just a number—it’s a warning sign that could mean your heart is at risk for dangerous rhythms. If this interval gets too long, your heart can skip, flutter, or even stop suddenly. It’s rare, but it’s real—and it’s often triggered by things you’re already taking.
Many common drugs can stretch your QTc interval without you knowing it. Antibiotics like azithromycin, antifungals like fluconazole, antidepressants like citalopram, and even some stomach meds like domperidone can do it. Even over-the-counter antihistamines like diphenhydramine have been linked to prolonged QTc in sensitive people. It’s not about being allergic—it’s about how your body handles the drug’s effect on heart cells. And if you’re already on more than one of these, or have kidney or liver issues, your risk goes up fast. You don’t need to panic, but you do need to know what’s in your medicine cabinet.
The good news? Doctors check for this all the time—especially before starting new meds or if you have a history of heart rhythm problems. An ECG is simple, painless, and often covered by insurance. If your QTc is borderline, they might switch your drug, lower the dose, or just monitor you closer. But if you’re taking something new and start feeling dizzy, faint, or notice your heart racing for no reason, don’t wait. That’s your body telling you something’s off.
What you’ll find below are real, practical guides from people who’ve been there. We’ve pulled together posts that show exactly which medications can mess with your QTc, how to spot the signs before it’s too late, and what to ask your pharmacist when you’re handed a new script. You’ll see comparisons of heart drugs that are safer, advice on checking for dangerous combos, and even how to read your own ECG report. This isn’t theory. It’s what works when your heart’s on the line.
- November 17, 2025
- Comments 6
- Medications and Supplements